Top Medication Safety Questions to Ask at the Pharmacy Counter

Every year, over 1.5 million people in the U.S. are harmed by medication errors. Many of these mistakes happen because patients don’t ask the right questions at the pharmacy. You’re not alone-nearly 4 out of 10 people leave the counter without fully understanding their new prescription. But a simple conversation with your pharmacist can prevent a hospital visit, a dangerous reaction, or even a life-threatening mistake.
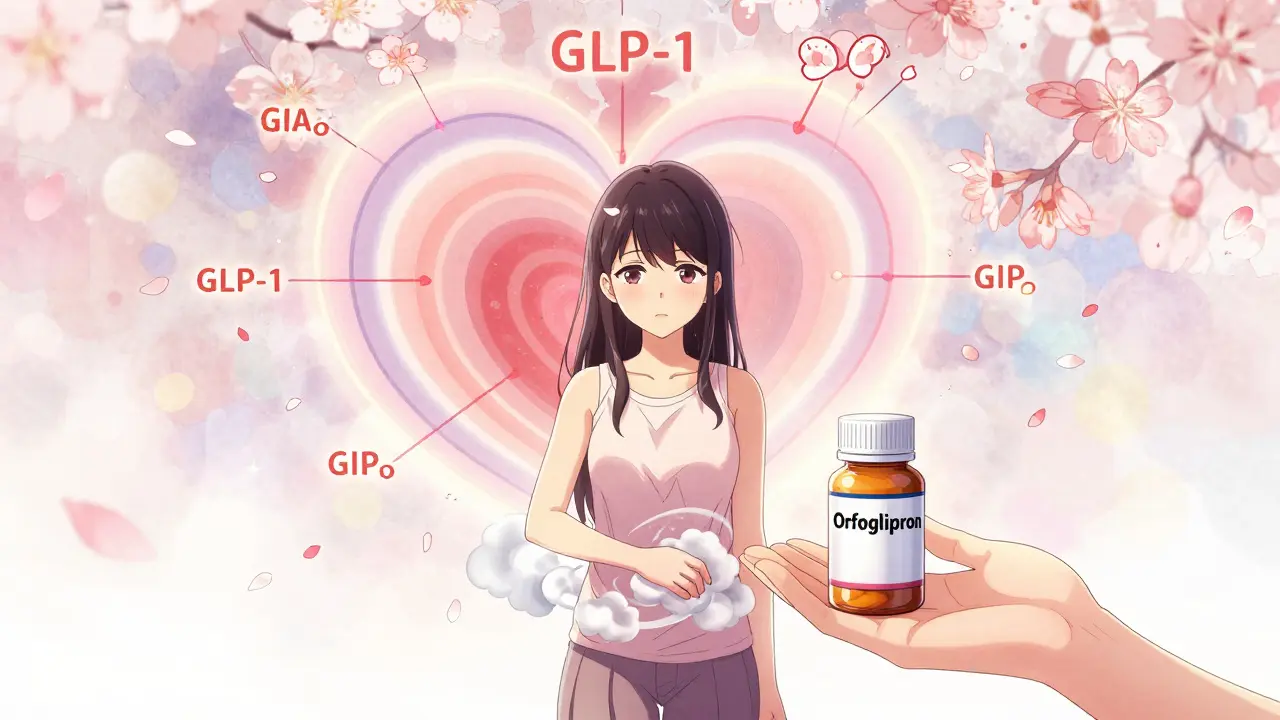
What is this medication for?
This is the most basic, yet most overlooked question. You might think you know why you’re taking it-your doctor said it’s for high blood pressure, or your friend uses it for migraines. But names can be confusing. Is this lisinopril or losartan? Both treat high blood pressure, but they work differently. Your pharmacist can confirm the exact condition it’s meant to treat and explain why it was chosen for you. If you’re unsure, ask: “Is this meant to treat my symptoms, or prevent something from getting worse?” Some medications, like statins or low-dose aspirin, are taken long-term to reduce risk-not to fix an immediate problem. Knowing the purpose helps you spot if something’s wrong later.
How and when should I take this?
“Take one by mouth daily” sounds simple-but what does that really mean? Should you take it with food? On an empty stomach? At night or in the morning? Some meds, like thyroid pills, must be taken alone, 30 to 60 minutes before breakfast. Others, like certain antibiotics, need to be spaced exactly 12 hours apart. If you take a pill with grapefruit juice, it could become dangerously strong. If you take a steroid with food, it might cause stomach upset. Your pharmacist can tell you the exact timing, whether to swallow whole or split, and if it’s safe to crush or chew. One patient in Texas accidentally crushed a slow-release pain pill, thinking it’d work faster. The result? A dangerous overdose. Always ask how to take it-not just how often.
What side effects should I watch for?
Not all side effects are created equal. Some are annoying but harmless-like dry mouth from an antihistamine. Others are red flags. If you’re on a blood thinner and start bruising easily, or if you’re taking an antidepressant and feel sudden thoughts of self-harm, you need to act fast. Ask your pharmacist: “Which side effects mean I should call you or go to the ER?” The FDA requires medication guides to list serious risks, but pharmacists can explain them in plain language. For example, if you’re on a statin, muscle pain isn’t just a nuisance-it could be a sign of rhabdomyolysis, a rare but dangerous condition. If you’re on a medication that makes you sensitive to sunlight-like some antibiotics or diuretics-you might burn faster than usual. Don’t assume it’s just “normal.” Ask what’s normal and what’s not.
Does this interact with anything else I take?
You might think your doctor knows everything you’re on-but most don’t. People take vitamins, herbal teas, over-the-counter painkillers, and even supplements like magnesium or melatonin without telling their prescriber. But these can clash. Ibuprofen with warfarin? That combination can raise your risk of stomach bleeding by up to 60%. St. John’s wort with antidepressants? That can trigger serotonin syndrome-a potentially fatal reaction. Even common things like calcium supplements can block absorption of thyroid meds. Bring every pill, bottle, and jar to the pharmacy. That includes eye drops, skin creams, and CBD oil. One patient in Pennsylvania was taking a blood pressure med and a popular herbal supplement for sleep. The pharmacist spotted the interaction and saved her from a dangerous drop in blood pressure. Don’t guess. Show them everything.
Is there anything in this that could cause an allergic reaction?
Allergies aren’t just to peanuts or penicillin. Some people react to dyes, fillers, or preservatives in pills. Red dye #40, lactose, or gluten can trigger rashes, swelling, or breathing trouble-even if you’ve never had an allergy before. Ask: “Does this contain any of these?” and name your known triggers. If you’ve ever had a rash from a medicine, even years ago, mention it. One man in Florida had a severe reaction to a generic version of his heart med because the new version used a different dye. He didn’t know the difference until his pharmacist pointed it out. Generic drugs have the same active ingredient, but not always the same inactive ones. That’s why it matters.
How should I store this?
Medications aren’t all meant to sit in your bathroom cabinet. Insulin? It goes in the fridge-unless you’re traveling, then it’s fine at room temperature for a few weeks. Antibiotics like amoxicillin? Once mixed, they can lose potency if left out too long. Some pills break down in heat or humidity. One pharmacist in Austin told of a patient who kept his blood pressure pills in his car’s glove compartment. By summer, the medication was ineffective. He ended up in the ER with dangerously high blood pressure. Check the label for storage instructions. If it says “refrigerate,” don’t ignore it. If it says “protect from light,” keep it in its original container. Don’t transfer pills to pill organizers unless you know it’s safe. Some meds are sensitive to air, moisture, or temperature changes.
Can I take this with my other health conditions?
Having diabetes, kidney disease, liver problems, or heart failure changes how your body handles drugs. A painkiller that’s fine for a healthy person might be risky if your kidneys aren’t working well. A sleep aid might make your breathing worse if you have sleep apnea. Your pharmacist reviews your full health history-not just your current meds. Ask: “Is this safe with my [condition]?” For example, if you have glaucoma, some cold medicines can raise eye pressure. If you’re on dialysis, certain antibiotics need dose adjustments. Even something as simple as a cough syrup can contain sugar or alcohol, which matters if you’re diabetic or recovering from addiction. Your pharmacist is trained to spot these hidden risks.
May I repeat back what you told me?
This one trick cuts communication errors by over 30%. After the pharmacist explains everything, say: “Let me repeat it back to make sure I got it right.” Then say it in your own words. “So you’re saying I take this pill every morning before breakfast, not with coffee, and if I get dizzy or see spots in my vision, I should call right away?” If they correct you, you just avoided a mistake. Pharmacists at Pocono Pharmacy started using this “teach-back” method in 2023-and saw a 44% drop in medication-related readmissions. It’s not about doubting them-it’s about making sure you understand. Most people don’t ask this because they’re embarrassed. But your pharmacist expects it. They’ve seen what happens when people don’t.
What if I miss a dose?
Life happens. You forget. You’re traveling. You’re sick. You skip a pill. What now? Some meds, like birth control or antibiotics, need strict timing. Others, like blood pressure pills, are more forgiving. If you miss one, should you double up? Take it right away? Wait until tomorrow? Asking this ahead of time saves panic later. For example, if you miss a dose of warfarin, doubling up could cause bleeding. But if you miss a dose of a diuretic, it’s usually fine to take it later the same day. Your pharmacist can give you a clear, written plan for missed doses. Keep it on your phone or taped to your pillbox.
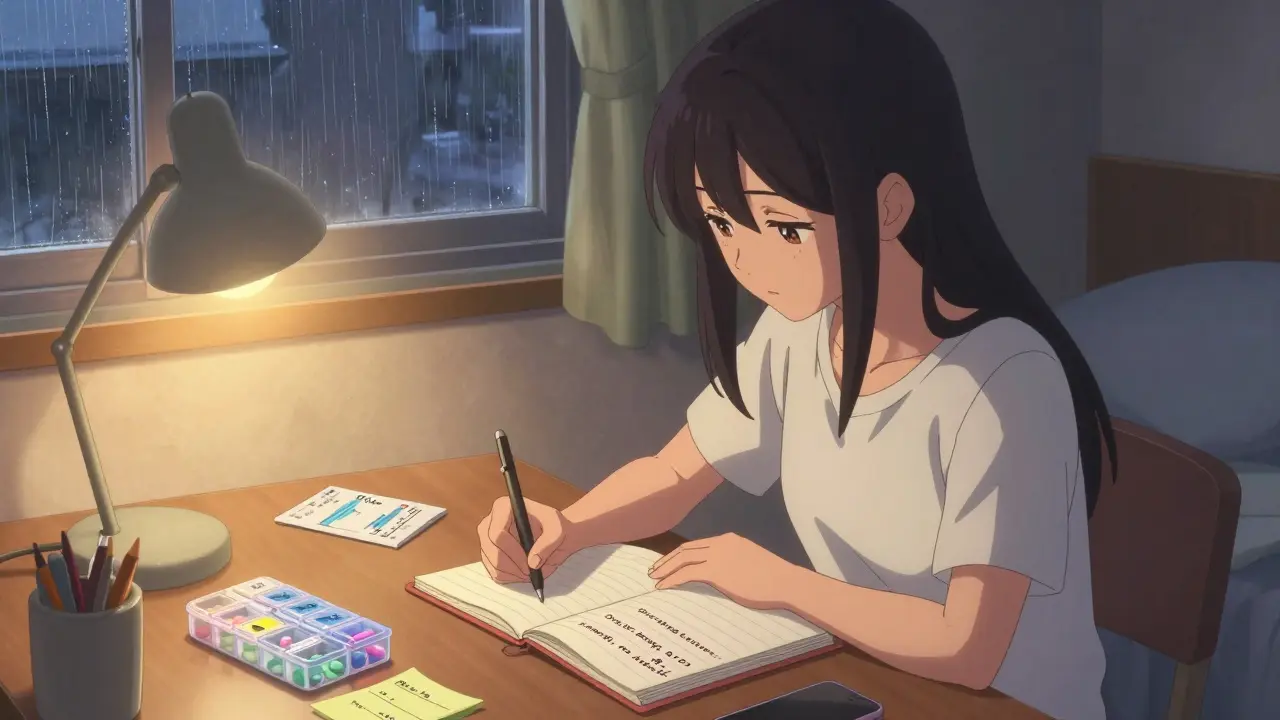
Can I get a written summary or medication list?
Most pharmacies can print out a list of all your current meds, including dosages, purposes, and instructions. Ask for it. Keep it in your wallet, phone, or with your medical records. This is especially important if you see multiple doctors or get hospitalized. Studies show that over half of hospital admissions involve medication errors-often because staff didn’t know what you were really taking. A printed list helps everyone stay on the same page. Some pharmacies even offer free digital copies via email or patient portals. Use it.
What if I have trouble swallowing or remembering to take it?
Many people stop taking meds because they’re hard to swallow or they forget. Don’t suffer in silence. Your pharmacist can help. They can suggest a liquid version, a different size pill, or a pill splitter. If you’re on multiple meds, ask about a blister pack or a dosing box with alarms. Some pharmacies even offer pre-filled weekly containers with your name and time labels on each compartment. One woman in Ohio had trouble remembering her 8 pills a day. Her pharmacist set up a weekly dispenser with color-coded sections and a reminder app. Her adherence jumped from 40% to 95%. There’s no shame in needing help. Pharmacists see this every day-and they’ve got solutions.
What should I do if I think something’s wrong?
Trust your gut. If you feel different after starting a new med-more tired, confused, nauseous, or just “off”-call your pharmacist. You don’t need to wait for a doctor’s appointment. Pharmacists are on the front lines. They can tell you if your symptoms match known side effects or if it’s something urgent. One man started a new cholesterol drug and felt his legs were heavy. He thought it was aging. His pharmacist recognized it as a rare side effect and told him to stop immediately. He avoided muscle damage. Don’t assume it’s normal. Don’t wait. Call.
Do I need to ask these questions every time I pick up a prescription?
Yes, especially if it’s a new medication or if the dosage or brand changed. Even if you’ve taken the same drug before, the formula, manufacturer, or your health status might have changed. Pharmacists check for new interactions every time. Never assume it’s the same.
What if I feel rushed at the pharmacy?
It’s okay to ask for a moment. Say: “I have a few quick questions about my meds-can we take two minutes?” Most pharmacists will pause. If they’re busy, ask to speak with them later, or request a phone call. Many pharmacies offer free 10-minute consultations by appointment. Don’t leave without clarity.
Can I ask about cheaper alternatives?
Absolutely. Pharmacists know which generics are available, which insurance tiers are cheaper, and even which programs offer discounts. They can often switch you to an equivalent drug that costs $10 instead of $100. Ask: “Is there a lower-cost option that works the same way?”
Should I ask about refills and expiration dates?
Yes. Know how many refills you have left and when the prescription expires. Some meds, like antibiotics or controlled substances, can’t be refilled after a certain date. Others, like insulin or liquid antibiotics, expire quickly after opening. Don’t use old meds. They lose strength or become unsafe.
Is it safe to take someone else’s leftover medication?
No. Even if it’s the same drug, the dose, formulation, or your health condition might be different. A pill that helped your friend’s headache could cause a dangerous reaction in you. Never share or reuse prescriptions. Dispose of unused meds properly at a pharmacy drop box.


Lisa Detanna
November 22, 2025 AT 19:17I used to think pharmacists were just there to hand out pills. Then my grandma had a bad reaction to a new blood pressure med because she didn’t ask about the dye. Turns out, the generic had red #40 and she’s allergic. I started asking every single question on that list-and now I print out the med list and bring it to every appointment. It’s not awkward, it’s lifesaving.
Pharmacists are the unsung heroes of healthcare. They catch errors doctors miss. They know what’s in your cabinet. They don’t judge. Just ask.
Stop being polite. Start being safe.
Demi-Louise Brown
November 24, 2025 AT 04:22Medication safety is a shared responsibility. Patients must be proactive. Pharmacists must be accessible. Systems must support clarity. This list is not optional. It is essential practice. Adherence improves outcomes. Communication prevents harm. Implement these steps. Protect yourself and those you love.
Matthew Mahar
November 25, 2025 AT 10:34OMG I JUST REALIZED I’VE BEEN KEEPING MY INSULIN IN THE BATHROOM CABINET FOR TWO YEARS. I THOUGHT IT WAS FINE BECAUSE THE BOTTLE SAID ‘STORE AT ROOM TEMP’ BUT I DIDN’T KNOW THAT MEANT ‘NOT IN A STEAMY HUMID HOLE’.
MY KID’S ASTHMA INHALER IS IN THE CAR GLOVEBOX TOO. I’M GOING TO THE PHARMACY TOMORROW AND I’M BRINGING EVERYTHING. EVERYTHING. I’M SCARED NOW BUT ALSO KIND OF PUMPED. THIS IS THE MOST IMPORTANT THING I’VE DONE FOR MY FAMILY IN YEARS.
John Mackaill
November 25, 2025 AT 15:54It’s interesting how few people realize pharmacists are trained clinicians, not just dispensers. In the UK, we’ve had pharmacist-led medication reviews for over a decade. Patients who use them report fewer side effects and better understanding. The barrier here seems to be cultural-we’re taught to defer to doctors, not question the system. But asking these questions isn’t defiance. It’s partnership.
Next time you’re at the counter, try saying: ‘Can we go through this together?’ You’ll be surprised how glad they are to help.
Casper van Hoof
November 26, 2025 AT 13:32The epistemological foundation of pharmaceutical safety rests upon the asymmetry of information between provider and recipient. The patient, often under stress, lacks the technical lexicon to interrogate the pharmacological intent of a prescribed agent. The pharmacist, as the final gatekeeper of therapeutic integrity, occupies a unique position of epistemic authority. To empower the patient is not merely to inform, but to reconstruct the power dynamic of care. This checklist, therefore, functions not as a procedural tool, but as a hermeneutic act of reclaiming agency in medical discourse.
Richard Wöhrl
November 26, 2025 AT 23:28Just a quick note: if you’re on warfarin, never take ibuprofen or naproxen without checking with your pharmacist-those NSAIDs can spike your INR and cause internal bleeding. Also, if you’re taking a statin and you start having unexplained muscle pain, especially in your thighs or shoulders, stop it immediately and call your pharmacist. Rhabdomyolysis is rare, but it’s real-and it can kill you in days if ignored.
And please, please, please don’t take your antibiotics with orange juice or milk. Some are absorbed way worse that way. And if you’re on thyroid meds, wait at least 30 minutes after taking it before you drink coffee or eat anything. I’ve seen people do this for years and wonder why their TSH is always off.
Pharmacists don’t get enough credit. They’re the ones who catch the 300mg dose that was supposed to be 30mg. They’re the ones who notice your new supplement is interacting with your heart med. Don’t be shy. Ask. Bring the list. Show them the bottles. They’ve seen it all. They’ll thank you.
Pramod Kumar
November 27, 2025 AT 00:30Bro, in India, we don’t even get this level of care. Pharmacies are just counters with bottles. You hand over the script, they hand you the pills, and you’re lucky if they say ‘take twice a day.’ No one asks about interactions, no one checks your other meds. I once saw a guy take his diabetes pill with milk tea-his sugar went nuts.
But here’s the thing: when I moved to the U.S. and asked my pharmacist about my cholesterol med, she pulled out a chart, showed me the side effects, and even printed a color-coded calendar for my pills. I cried. Not because I was sick-but because someone actually cared enough to explain.
Don’t take this for granted. Ask. Even if you feel dumb. You’re not dumb-you’re smart for asking.
Brandy Walley
November 28, 2025 AT 23:51Ugh. So now we’re supposed to interrogate every pharmacist like they’re a suspect? I mean, I get it, but this feels like medical paranoia. My doctor knows what they’re doing. If I had a bad reaction, I’d go back. Why overcomplicate it? Also, I don’t carry my meds to the pharmacy-I just show the bottle. And why would I repeat back what they say? Like I’m in kindergarten?
Also, why do you assume everyone has time for 10-minute consultations? I work two jobs. My meds are fine. Stop shaming people for not being perfect patients.
shreyas yashas
November 29, 2025 AT 21:23My aunt took her meds wrong for months because she thought ‘once daily’ meant ‘whenever I remember.’ She ended up in the hospital. Now I use a pill box with alarms. My pharmacist even set up a WhatsApp reminder for her. No fancy app, just a simple message every morning at 8.
And yeah, she’s 78. Doesn’t matter. We all forget. We all get confused. The pharmacy isn’t the enemy. Silence is. Ask. Even if you’re scared. Even if you think it’s dumb. You’re not dumb. You’re alive. And that’s worth two minutes of your time.