Next-Generation GLP-1 Agents: What You Need to Know About Safety and Side Effects
GLP-1 Weight Loss Estimator
How This Tool Works
This estimator uses clinical trial data to provide approximate weight loss expectations. Results are based on typical patient outcomes and should not replace professional medical advice. Actual results may vary based on individual factors.
Select Your GLP-1 Agent
Personalize Your Estimate
When you hear about GLP-1 agonists, you might think of weight loss miracles. And yes, these drugs have changed the game. But behind the headlines and social media buzz lies a more complicated story - one about safety, tolerability, and what’s really happening in the body when you take them. The next generation of GLP-1 agents isn’t just stronger. It’s different. And that changes everything about how they affect you.
What Are Next-Generation GLP-1 Agents?
GLP-1 receptor agonists were first developed to help people with type 2 diabetes control their blood sugar. But doctors quickly noticed something surprising: patients lost weight. A lot of it. That led to a whole new wave of research. Today’s GLP-1 drugs aren’t just mimicking one hormone anymore. They’re engineered to hit multiple targets at once.
Take retatrutide a triple agonist that activates GLP-1, GIP, and glucagon receptors. In Phase II trials, people lost up to 24.2% of their body weight after 48 weeks. That’s not a typo. Compare that to the first-generation drugs like liraglutide, where weight loss averaged around 5-7%. Then there’s orforglipron the first oral GLP-1 agonist to show strong results in trials, with patients losing 15-20% of body weight over time. Even VK2735 a dual GLP-1/GIP agonist in oral form hit nearly 15% weight loss in just 13 weeks.
These aren’t just improved versions. They’re fundamentally different drugs. They’re designed to last longer, work better, and be taken more easily - especially oral versions like orforglipron. But with greater power comes greater complexity in how your body responds.
Side Effects: It’s Still Mostly Gut Issues
Here’s the thing: no matter how advanced these new drugs are, your stomach still complains. A lot.
Studies from the 2025 American Diabetes Association Standards of Care show that 30-50% of people on traditional GLP-1 drugs like semaglutide or liraglutide experience nausea, vomiting, diarrhea, or constipation. And guess what? The next-gen agents aren’t fixing that. In fact, a 2025 study published in PubMed (PMID: 40685266) found that dual and triple agonists like retatrutide and VK2735 cause just as many gastrointestinal side effects as the older ones.
That’s surprising. You’d think adding GIP or glucagon into the mix might calm things down. But it doesn’t. Nausea is still the #1 reason people stop taking these drugs. Around 5-10% of patients quit because the side effects are too intense - especially at higher doses. And those doses are where the biggest weight loss happens.
Orforglipron’s safety profile is similar: mild to moderate GI issues, mostly during the first few weeks. The good news? Most people get used to it. About 70-80% of users report that nausea and stomach discomfort fade within 4 to 8 weeks if they stick with the treatment. The key? Slow titration. Jumping straight to the highest dose? That’s a recipe for discomfort. Doctors now recommend taking 16 to 20 weeks to reach the full maintenance dose.
What’s Not Being Talked About: Muscle, Bone, and Long-Term Risks
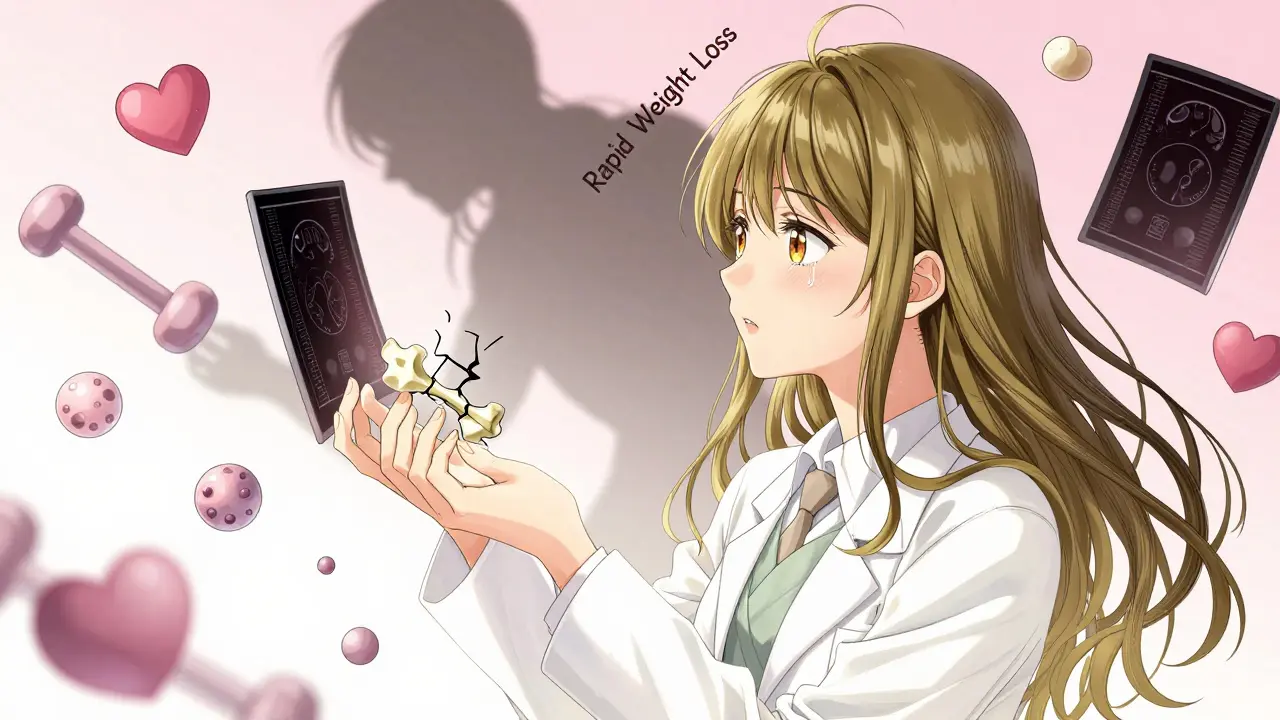
Everyone talks about weight loss. But what happens to your muscle? Your bones? Your metabolism over five years?
Dr. Daniel J. Drucker, a leading researcher at the University of Toronto, warns that rapid weight loss - especially over 20% - can threaten muscle mass. When you lose weight this fast, your body doesn’t always distinguish between fat and muscle. Without intentional resistance training and adequate protein intake, you could lose more muscle than you realize.
The American Gastroenterological Association also flags a lingering concern: pancreatitis. While the risk is low, it hasn’t been fully ruled out. Long-term data doesn’t exist yet for drugs that cause 20%+ weight loss. We don’t know how they affect liver function, kidney health, or gallbladder function over 5, 10, or 15 years.
And then there’s bone density. A 2025 review in the Diabetes Journal noted that sustained, extreme weight loss may impact bone mineral density, especially in postmenopausal women and older adults. No one’s saying these drugs are dangerous - but we’re flying blind in some areas. The FDA’s upcoming Phase III trials for retatrutide are now including detailed assessments of musculoskeletal health, bone scans, and nutritional markers. That’s a sign they know we’re missing answers.
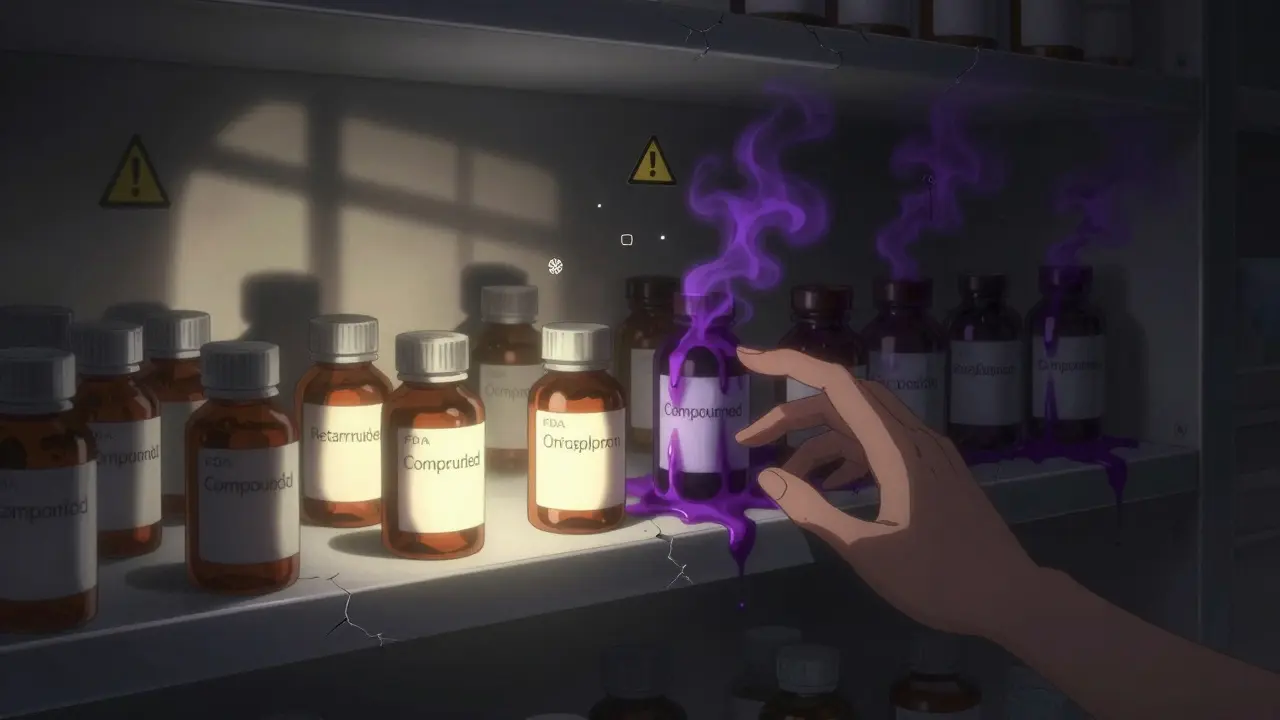
The Compounded Drug Problem
Here’s where things get dangerous.
Online pharmacies and compounding clinics are selling fake versions of semaglutide, tirzepatide, and other GLP-1 drugs. They’re cheaper. They’re easy to get. And they’re risky.
The University of Illinois at Chicago’s Digital Pharmacy issued a blunt warning in August 2025: compounded GLP-1 products have 3 to 5 times higher rates of adverse events than FDA-approved versions. Why? Dosing errors. Contaminants. Unstable formulations. One patient reported severe vomiting and dizziness after taking a compounded version that turned out to have 40% more active ingredient than labeled.
The FDA has issued multiple alerts since 2024. They’re not just warning consumers - they’re cracking down on labs that don’t follow USP <795> standards. If you’re considering a non-FDA-approved version, ask your doctor to verify the pharmacy. Ask for batch numbers. Ask for certificates of analysis. If they can’t provide them, walk away.
Oral vs. Injectable: The Real Trade-Off
Orforglipron is the first oral GLP-1 agonist to show real promise. That’s huge. No more needles. No more storage. No more travel restrictions.
But here’s the catch: oral drugs have to survive your stomach acid, get absorbed through your gut, and still reach enough concentration in your bloodstream to work. That’s why orforglipron’s doses are so high - 6mg, 12mg, even 36mg. And even then, its side effect profile is nearly identical to injectables.
So is oral better? For some, yes. If you hate needles, it’s a game-changer. But if you’re looking for fewer side effects? No. The data shows the same nausea, same vomiting, same diarrhea. The advantage is convenience, not comfort.
Who Should Avoid These Drugs?
These aren’t magic pills. They’re powerful tools - and they’re not for everyone.
- People with a personal or family history of medullary thyroid cancer or multiple endocrine neoplasia syndrome - GLP-1 drugs carry a black box warning for thyroid C-cell tumors in rodents, and while human risk isn’t confirmed, the caution remains.
- Those with a history of severe GI disorders like gastroparesis or chronic pancreatitis - slowing gastric emptying could make things worse.
- People with very low body weight or a history of eating disorders - rapid weight loss can trigger relapse or nutritional collapse.
- Anyone taking insulin or sulfonylureas - combining these with GLP-1 drugs increases hypoglycemia risk unless doses are adjusted carefully.
And if you’re pregnant, planning to get pregnant, or breastfeeding? These drugs aren’t approved. Stop them at least two months before trying to conceive. The long half-life means they linger in your system.
What’s Coming Next?
Retatrutide’s Phase III results are due by late 2025. If they’re as strong as Phase II, the FDA could approve it by mid-2026. That’s the first triple agonist likely to hit the market.
Viking Therapeutics is pushing VK2735 into Phase III trials. Merck’s danuglipron is also in late-stage testing. And the race is on for a once-weekly oral version - something that would be a true revolution.
But the real breakthrough won’t be another drug. It’ll be personalized use. Researchers are now looking at metabolic phenotypes - not just BMI - to match patients with the right drug. Someone with high insulin resistance might respond better to a GLP-1/GIP combo. Someone with low muscle mass might need a triple agonist with added glucagon to preserve lean tissue.
For now, the message is simple: these drugs work better than ever. But they’re not risk-free. Your body isn’t just losing fat. It’s adapting to a major metabolic shift. That takes monitoring, patience, and smart care.
Are next-generation GLP-1 agents safer than older ones?
Not necessarily. While they’re more effective at weight loss, their side effect profile - especially gastrointestinal issues like nausea and vomiting - is similar to older drugs. The biggest safety difference lies in compounded versions, which are far riskier than FDA-approved products. Long-term risks like muscle loss, bone density changes, and organ strain are still being studied.
Can I take oral GLP-1 drugs if I’ve had trouble with injections?
Yes - oral versions like orforglipron are designed for people who dislike injections. But don’t expect fewer side effects. The nausea, bloating, and stomach upset are just as common. The benefit is convenience, not comfort. Talk to your doctor about whether your digestive system can handle the higher doses needed for oral absorption.
Why do I still get nausea even after months on the drug?
If nausea lasts longer than 8 weeks, it could mean your dose is too high, you’re not eating enough protein, or your body isn’t adapting. Some people are simply more sensitive to GLP-1 effects. Talk to your provider about holding your dose longer, switching to a different agent, or adding a slow-release anti-nausea medication like low-dose ondansetron. Never stop abruptly - this can cause rebound weight gain and blood sugar spikes.
Is it safe to use compounded GLP-1 drugs if they’re cheaper?
No. Compounded versions lack FDA oversight and often have inconsistent dosing, contaminants, or incorrect ingredients. The University of Illinois at Chicago reported 3-5 times more adverse events from compounded products. One patient ended up in the ER after a compounded semaglutide dose was 40% too high. Stick to FDA-approved brands - even if they cost more, the risk isn’t worth it.
Do these drugs affect muscle mass?
Yes, especially with rapid weight loss over 20%. Studies suggest up to 25% of weight lost may come from muscle, not fat, without proper intervention. To protect muscle: eat 1.6-2.2 grams of protein per kilogram of body weight daily, lift weights at least twice a week, and consider checking your body composition with a DEXA scan after 6 months. Retatrutide trials now include muscle mass tracking - because it’s a real concern.
Final Thoughts
These drugs are revolutionary. But they’re not magic. They’re medicine - powerful, precise, and demanding careful use. The biggest mistake people make is thinking more weight loss equals better results. It doesn’t. It just means more strain on your body. If you’re considering one of these agents, don’t chase the highest dose. Chase the right one. Work with your doctor to find the balance between effectiveness and safety. And if you’re tempted by a cheaper, online version? Don’t. The risks aren’t worth the savings.