Oncology and Cancer: Practical Guide to Capecitabine
Capecitabine is an oral chemotherapy many patients meet sooner or later. It turns into 5‑fluorouracil (5‑FU) in the body and targets fast‑growing cancer cells. Because you can take it at home, capecitabine changes how treatment fits into daily life — but it brings specific risks and routines worth knowing.
How capecitabine works and when it's used
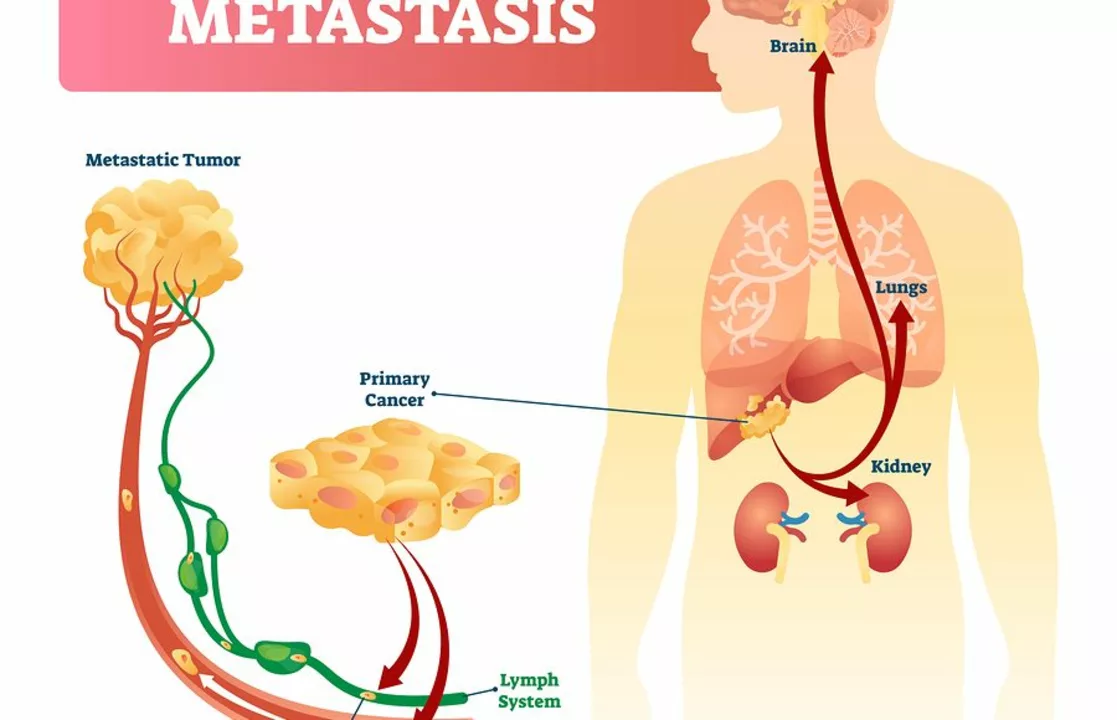
Doctors prescribe capecitabine for metastatic breast cancer and colorectal cancer, and sometimes with other drugs like oxaliplatin (CAPOX) or with radiation. The drug is a prodrug, meaning it converts into the active chemo inside tissues. That helps concentrate the effect where tumors are more active.
Oral dosing can be more convenient than IV chemo, but it also means you must stick to a schedule, track pills, and report side effects quickly. Many patients prefer taking pills to frequent clinic infusions, but the responsibility for correct daily use shifts to you and your caregiver team.
Practical tips: monitoring and managing side effects
Capecitabine can lower white blood cells, which raises infection risk. Your healthcare team will order regular blood counts. If you get a fever, chills, or signs of infection, contact them immediately — fevers during chemo need fast attention.
Hand‑foot syndrome (redness, swelling, and pain on palms and soles) is common. Keep skin moisturized, avoid hot water and tight shoes, and use cushioning in shoes. If redness or blisters appear, call your clinic; dose changes often prevent worse problems.
Diarrhea and mouth sores also happen. Stay hydrated, eat bland foods, and tell your care team early so they can recommend medicines and adjust doses. Some patients need dose reductions to stay safe while keeping benefit.
Capecitabine is processed partly by the liver and kidneys. Blood tests check liver enzymes and kidney function because changes can affect how the drug is cleared. A small number of people have severe reactions due to DPD enzyme deficiency; some centers test for DPD before treatment to prevent life‑threatening toxicity.
Take capecitabine within 30 minutes after a meal, usually twice a day for two weeks followed by a one‑week break in many common schedules. Exact timing and length vary by regimen; follow your oncologist’s plan and double‑check with the pharmacy if unsure.
Avoid pregnancy during treatment and use effective contraception. Capecitabine can harm a fetus. Men and women should discuss fertility preservation before starting treatment if that’s a concern.
Combining capecitabine with other drugs can raise specific side effects. For example, when paired with oxaliplatin, patients may see more nerve symptoms. Your team will explain the likely side effects for your exact regimen and how they’ll monitor you.
Simple habits help: keep a medication calendar, bring all drugs to clinic visits, report new symptoms early, and ask for written instructions about dose changes. Good communication with nurses and pharmacists reduces surprises and keeps treatment on track.
If you want more detail about a specific regimen or side effect, ask your oncology team or pharmacist. They can tailor advice to your health, other meds, and test results so you get the safest and most effective care.
Cancer Prevention: How Lifestyle and Chemoprevention Reduce Your Risk
Cancer prevention through lifestyle changes like quitting smoking, staying active, eating vegetables, and limiting alcohol can reduce your risk by up to 40%. Chemoprevention may help high-risk individuals but isn't for everyone. Start with one small habit today.
VIEW MOREMultiple Myeloma: Understanding Bone Disease and the New Drugs Changing Outcomes
Multiple myeloma causes severe bone damage in over 80% of patients. New drugs like romosozumab and DKN-01 are now showing promise in healing bone lesions, not just preventing them. Learn how these novel agents are changing treatment.
VIEW MOREBrain Tumors: Types, Grades, and Multimodal Treatments Explained
Brain tumors are classified by type, grade, and molecular markers. Understanding WHO CNS5 grading and treatments like vorasidenib helps patients and doctors make smarter, personalized decisions for better outcomes.
VIEW MOREChemotherapy Hypersensitivity Reactions: Signs, Risks, and What to Do Immediately
Chemotherapy hypersensitivity reactions can range from mild itching to life-threatening anaphylaxis. Learn the key signs, high-risk drugs, emergency protocols, and how to prevent or respond to these reactions safely.
VIEW MOREBasal vs. Squamous Cell Carcinoma: What You Need to Know About Nonmelanoma Skin Cancer
Basal and squamous cell carcinomas are the two most common types of nonmelanoma skin cancer. Learn how they differ in appearance, risk, treatment, and danger-so you can spot them early and protect your health.
VIEW MORELymphoma and Yoga: Benefits, Safety Tips & Practice Guide
Explore how gentle yoga can ease lymphoma symptoms, boost immunity, and improve quality of life. Get safe practice tips, a sample routine, and answers to common questions.
VIEW MOREAnastrozole in Endocrine Therapy: Benefits, Risks, and Patient Guide
Clear, evidence-based guide to anastrozole in endocrine therapy: who benefits, real-world risks, dosing, side-effect fixes, and how it compares to tamoxifen and other AIs.
VIEW MOREThe role of capecitabine in the management of metastatic cancer
As a blogger, I've recently researched the role of capecitabine in the management of metastatic cancer. Capecitabine is an oral chemotherapy drug that has proven to be effective in treating various types of metastatic cancers, including breast and colorectal cancer. It works by inhibiting the synthesis of DNA in cancer cells, ultimately slowing down or stopping their growth. The convenience of taking capecitabine orally, as opposed to intravenous chemotherapy, has been a game-changer for cancer patients, allowing them to receive treatment in the comfort of their own homes. Overall, capecitabine has become a critical component in managing metastatic cancer and improving patients' quality of life.
VIEW MOREThe impact of capecitabine on the immune system
As a copywriter, I've recently been researching the impact of capecitabine on the immune system. Capecitabine is a chemotherapy drug that's often used to treat various types of cancer. From my understanding, it can weaken the immune system by reducing the number of white blood cells, making it harder for the body to fight infections. However, it's essential to know that the drug's impact on the immune system varies from person to person. In any case, it's crucial for patients on capecitabine to be closely monitored by their healthcare team to manage potential side effects and maintain a healthy immune system.
VIEW MORE