Basal vs. Squamous Cell Carcinoma: What You Need to Know About Nonmelanoma Skin Cancer

What Are Basal and Squamous Cell Carcinomas?
Nonmelanoma skin cancer isn’t one disease-it’s two. Basal cell carcinoma and squamous cell carcinoma make up 95% of all nonmelanoma skin cancers. Together, they’re the most common cancers in humans. More than 5.4 million cases are diagnosed in the U.S. every year. Most people don’t realize how different these two cancers are, even though they look similar at first glance.
Basal cell carcinoma starts in the deepest layer of your epidermis, where new skin cells are born. It grows slowly and rarely spreads. Squamous cell carcinoma begins in the top layer of skin, where cells flatten out as they rise to the surface. It’s less common but more dangerous because it can spread to other parts of the body if ignored.
How Do They Look Different?
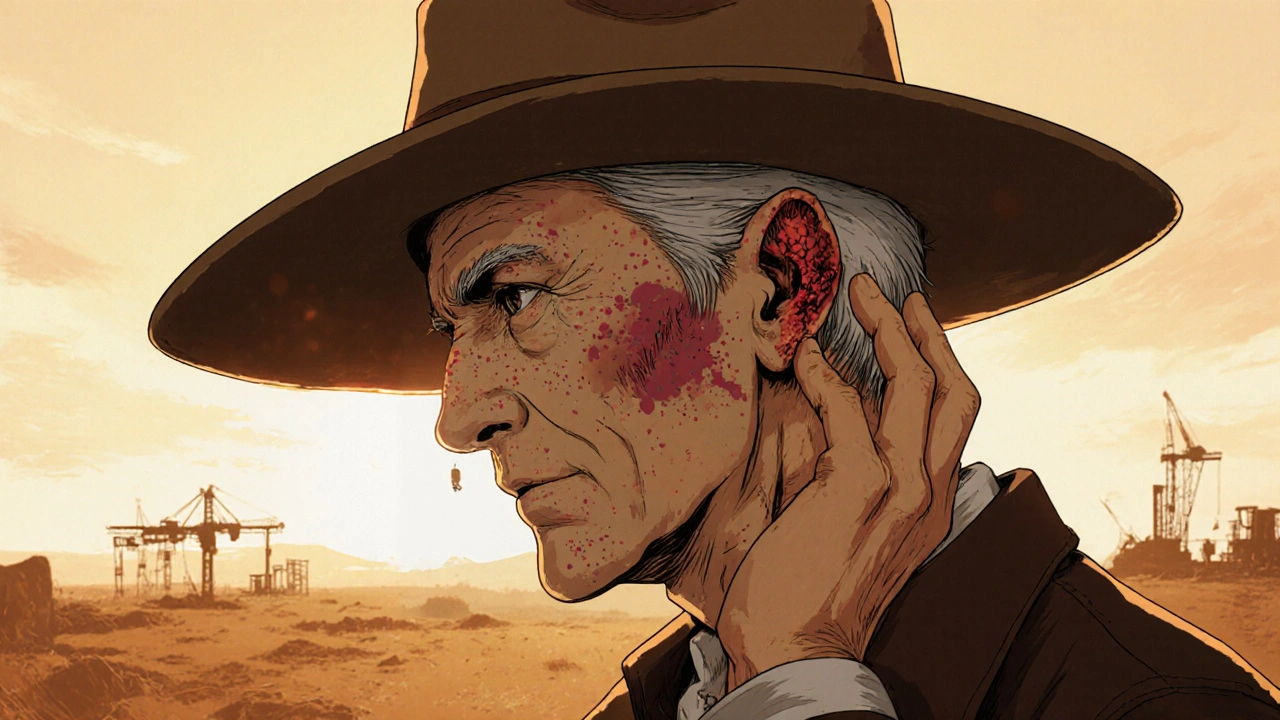
Knowing what to look for can save your life. Basal cell carcinoma often shows up as a shiny, pearly bump-like a tiny pearl under the skin. It might also look like an open sore that bleeds, oozes, or crusts over but never fully heals. Sometimes, it appears as a flat, scar-like patch that’s white or yellow. These are most common on the face, ears, and neck.
Squamous cell carcinoma looks different. It’s usually a firm, red bump that feels rough or scaly. It can look like a wart, or a flat, reddish patch that grows slowly. Unlike BCC, SCC often crusts or bleeds easily. You might notice it on your hands, arms, scalp, or lips. If you see a sore that doesn’t heal in 4-6 weeks, especially if it’s growing or changing fast, get it checked.
Who’s at Risk?
Both cancers are tied to sun exposure, but in different ways. Basal cell carcinoma is often linked to intense, intermittent sunburns-like a bad weekend at the beach or a childhood sunburn that blistered. Squamous cell carcinoma is more about lifelong, cumulative exposure. Think farmers, construction workers, or anyone who’s spent decades outside without protection.
Age matters. Eighty-five percent of cases happen in people over 50. The average age of diagnosis is 67 for BCC and 69 for SCC. Fair skin, light eyes, and blonde or red hair raise your risk. But it’s not just about skin tone. People who’ve had organ transplants are 250 times more likely to develop SCC than the average person. That’s because immunosuppressant drugs weaken the body’s ability to fight off cancer cells.
Men are more likely to get SCC-65% of cases occur in men, compared to 55% for BCC. That’s likely because of occupational sun exposure. Women get more BCC, possibly because of more frequent cosmetic sun exposure.
Which One Is More Dangerous?
Basal cell carcinoma is the most common-but squamous cell carcinoma is the more serious one. Here’s why: BCC almost never spreads. Fewer than 0.1% of cases metastasize. Even when left untreated for years, it mostly just eats away at local tissue-destroying skin, cartilage, or bone in the face or ear.
SCC is different. It metastasizes in 2-5% of cases. That might sound low, but it’s 10 times more likely than BCC. When it spreads, survival rates drop from 95% to 25-45%. High-risk spots like the lips, ears, and genitals have even higher spread rates-up to 14% for lip SCC. That’s why doctors treat SCC more aggressively from the start.
Dr. John Zitelli, former president of the American College of Mohs Surgery, says it plainly: “While basal cell carcinoma is more common, squamous cell carcinoma requires more urgent attention.”
Treatment Differences
Both cancers are highly curable if caught early. Surgical removal works for both, with cure rates above 95%. But the approach changes based on the type.
For early, superficial BCC, topical creams like imiquimod or 5-fluorouracil can clear up to 70% of cases. That’s rare with SCC-topical treatments only work about 40-50% of the time. That’s because SCC grows deeper faster.
Mohs surgery is the gold standard for both. It removes cancer layer by layer while checking margins under a microscope. It cures 99% of primary BCC and 97% of primary SCC. But SCC often needs wider excision margins-4-10 mm compared to 3-5 mm for BCC. That means more skin removed, and sometimes more reconstructive surgery.
Patients with SCC need more follow-ups. On average, they have 2.3 times more appointments than BCC patients. Why? Because SCC is more likely to come back. In immunocompromised people, recurrence rates hit 15% for SCC versus 5% for BCC.
Prevention and Early Detection
Sun protection is your best defense. Daily sunscreen use reduces BCC risk by 40% and SCC risk by 50%. That’s because SCC is more directly tied to long-term UV damage. Wearing hats, avoiding midday sun, and skipping tanning beds matter more for SCC.
Self-checks are critical. Look for new growths, sores that won’t heal, or spots that change in size, color, or texture. Use the ABCDE rule for melanoma, but for nonmelanoma cancers, focus on: Non-healing, Fast-growing, Crusting or bleeding.
High-risk people-those with past skin cancer, organ transplants, or fair skin-should see a dermatologist every 3-4 months. SCC often returns within 12 months of treatment. BCC takes longer, usually 18 months or more.

What’s New in Treatment?
Science is catching up. In 2018, the FDA approved cemiplimab-rwlc (Libtayo), the first immunotherapy drug for advanced SCC. It works in nearly half of metastatic cases where chemotherapy failed. For BCC, drugs like vismodegib target the hedgehog pathway and work in up to 85% of advanced cases.
Researchers at Johns Hopkins found that 90% of SCC tumors have TP53 gene mutations, compared to only 50% of BCC tumors. That explains why SCC is more aggressive and harder to control.
AI tools are helping dermatologists spot the difference. New dermoscopy apps are 94% accurate at telling BCC apart from SCC-faster and more reliably than the human eye alone.
What Patients Say
Real-world experiences show clear emotional and physical differences. On Reddit, 78% of SCC patients reported rapid growth of their lesions-compared to just 32% of BCC patients. Eighty-five percent of SCC patients worried about metastasis; only 42% of BCC patients did.
On RealSelf, 63% of SCC patients said treatment was painful; only 87% of BCC patients said it was “minimal pain.” That’s because SCC often requires deeper surgery, wider removal, and more complex reconstruction.
Patients with SCC on the face or ear are more likely to need skin grafts or flap surgery. One woman in Austin described her SCC removal on the ear as “losing part of my identity.” She needed a skin graft from her collarbone. BCC patients, even with facial removals, often heal with minimal scarring.
Bottom Line: Don’t Wait
Both basal and squamous cell carcinomas are treatable. But treating them early makes all the difference. BCC is a slow-moving problem. SCC is a ticking clock. One might look like a harmless bump. The other might look like a scab that won’t go away. But they’re not the same.
If you’ve had one skin cancer, you’re at higher risk for another. Get checked yearly-even if you think you’re “just being careful.” Sun damage adds up. And the longer you wait, the more damage it does.
Protect your skin. Know the signs. Act fast. Your skin is your largest organ. Treat it like it matters-because it does.
Can basal cell carcinoma turn into squamous cell carcinoma?
No, basal cell carcinoma cannot turn into squamous cell carcinoma. They come from different types of skin cells and develop independently. Having one does not mean you’ll develop the other-but it does mean your skin has been damaged enough to be at risk for both. People who’ve had one nonmelanoma skin cancer are more likely to get another, whether it’s BCC or SCC.
Is squamous cell carcinoma more dangerous than melanoma?
No, melanoma is far more dangerous. While SCC can spread and is the second leading cause of skin cancer deaths after melanoma, melanoma is much more aggressive. Melanoma has a higher rate of metastasis and is responsible for over 75% of skin cancer deaths, despite being less common. SCC is serious, but melanoma is the deadliest form of skin cancer.
Can I treat basal cell carcinoma with over-the-counter creams?
Some superficial basal cell carcinomas can be treated with prescription topical creams like imiquimod or 5-fluorouracil, but these are not available over-the-counter. You need a doctor’s diagnosis first. Self-treating with OTC products can delay proper care and allow the cancer to grow deeper. Always get a professional evaluation before starting any treatment.
How often should I get a skin check if I’ve had nonmelanoma skin cancer before?
If you’ve had one nonmelanoma skin cancer, you should see a dermatologist every 6 to 12 months. If you’ve had SCC, especially if it was high-risk or you’re immunocompromised, every 3 to 6 months is recommended. Recurrence is common-73% of SCC cases return within a year. Early detection saves lives.
Does sunscreen prevent both types of skin cancer equally?
No. Daily sunscreen use reduces the risk of basal cell carcinoma by about 40% and squamous cell carcinoma by about 50%. That’s because SCC is more strongly linked to long-term, cumulative sun exposure, while BCC is often tied to intense, intermittent burns. Still, sunscreen is your best defense against both. Use SPF 30 or higher, reapply every two hours, and don’t forget your ears, lips, and hands.

Neoma Geoghegan
November 23, 2025 AT 16:24Early = easy. Late = nightmare.
Bartholemy Tuite
November 24, 2025 AT 04:30Sam Jepsen
November 25, 2025 AT 14:53Yvonne Franklin
November 27, 2025 AT 12:03New Yorkers
November 27, 2025 AT 13:02Nikhil Chaurasia
November 28, 2025 AT 23:41Holly Schumacher
November 30, 2025 AT 17:04Melvina Zelee
December 2, 2025 AT 02:33ann smith
December 2, 2025 AT 21:15