Safe Use of Multiple Medications: How to Avoid Dangerous Double Ingredients
Every year, tens of thousands of people end up in the emergency room not because of a fall, infection, or heart problem-but because they took two different pills that contained the exact same active ingredient. It sounds impossible, right? But it happens more often than you think. You’re taking a prescription painkiller for your back. You grab a cold medicine off the shelf because you feel stuffy. You don’t realize both contain acetaminophen. By the time you feel dizzy or nauseous, your liver is already under stress. This isn’t a rare mistake. It’s a common, preventable crisis.
What Are Double Ingredients-and Why Do They Matter?
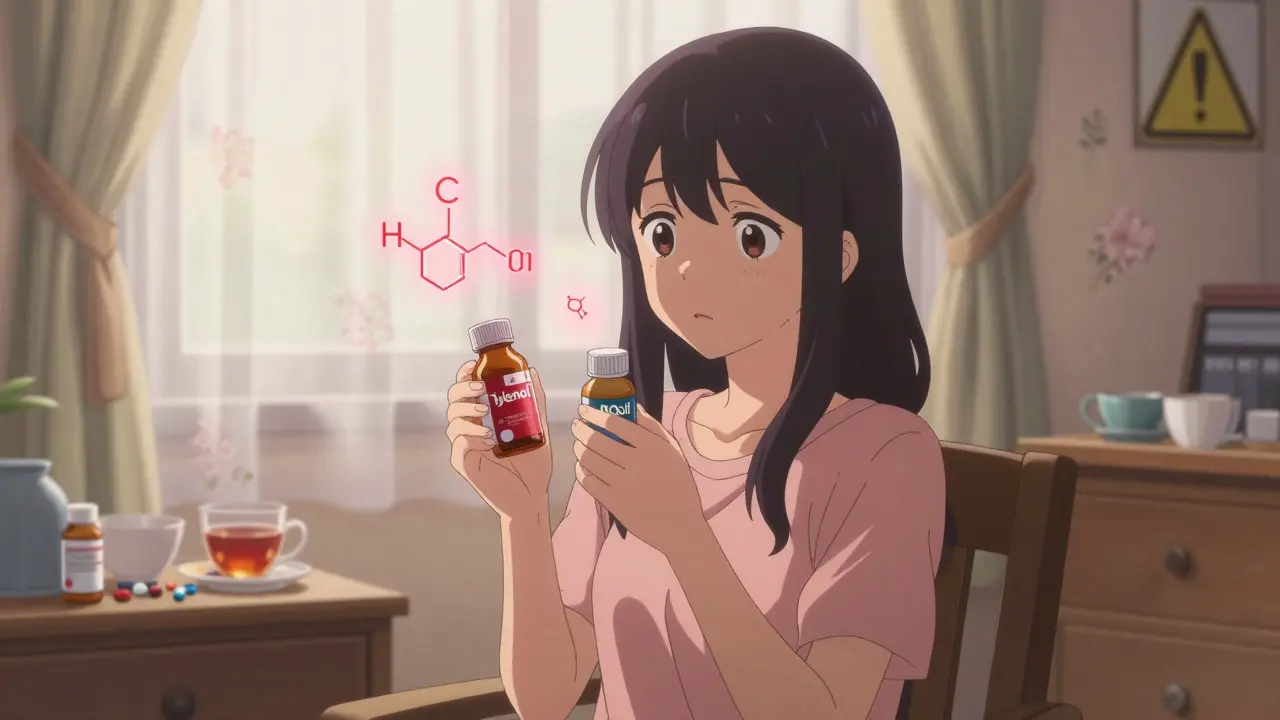
Double ingredients happen when you take two or more medications that contain the same active chemical. It’s not about drug interactions. It’s about duplication. You might think you’re being careful by using a prescription and an over-the-counter (OTC) product together, but you’re actually doubling your dose without knowing it. The most dangerous example? Acetaminophen. Found in Tylenol, Vicodin, Percocet, NyQuil, Excedrin, and dozens of other cold, flu, and pain products, it’s the leading cause of accidental liver failure in the U.S. The National Institutes of Health reports that more than 56,000 emergency room visits each year come from unintentional acetaminophen overdose. And most of those cases? People didn’t know they were taking it twice.Who’s Most at Risk?
Older adults are the most vulnerable. About 40% of people over 65 take five or more medications regularly-a condition called polypharmacy. The CDC says adults 65 and older make up 65% of all hospitalizations from double ingredient errors. Why? Because they often see multiple doctors, fill prescriptions at different pharmacies, and take OTC meds for arthritis, sleep, or congestion without telling anyone. A 2022 MedlinePlus survey found that 32% of people taking five or more meds have accidentally taken duplicate ingredients. And 61% have experienced symptoms like dizziness, extreme sleepiness, or stomach bleeding from it. But it’s not just seniors. Anyone taking multiple prescriptions, OTC drugs, or supplements is at risk. If you’re on blood pressure pills, a sleep aid, and a daily pain reliever, you’re already stacking ingredients. And if you’re also using herbal teas, CBD oils, or traditional remedies? That’s another hidden layer most doctors never ask about.The Hidden Culprits: Common Double Ingredient Traps
Some ingredients are so common, they’re practically invisible on labels. Here are the top three offenders:- Acetaminophen: Found in over 600 prescription and OTC products. Even if you only take one Tylenol a day, your painkiller or cold medicine might add another 500-1,000 mg. The safe daily limit is 3,000-4,000 mg, but many people cross it without realizing.
- Diphenhydramine: An antihistamine in Benadryl, Unisom, NyQuil, and some sleep aids. It causes drowsiness, confusion, and dry mouth. When combined with other sedatives like benzodiazepines or sleep prescriptions, it can lead to falls, delirium, or even breathing problems.
- NSAIDs: Ibuprofen and naproxen show up in Advil, Aleve, Excedrin, and many arthritis or menstrual pain formulas. Taking two NSAIDs at once-say, one for back pain and another for a headache-raises your risk of stomach bleeding and kidney damage.
And here’s the kicker: 45% of prescription labels don’t clearly warn you if the same ingredient is in OTC products. The FDA tried to fix this with standardized Drug Facts labels on OTC packages since 2020. But a 2023 government report found 41% of people still can’t spot duplicate ingredients on those labels.

Why Your Doctor Might Not Know
Most doctors focus on one condition at a time. If you’re seeing a cardiologist for blood pressure, a rheumatologist for arthritis, and a neurologist for migraines, each one prescribes what they think you need. But none of them know what you’re taking from the pharmacy shelf. Electronic health records rarely include OTC meds unless you tell them. And even then, many patients forget-or assume it’s not important. A 2021 study in the Journal of the American Geriatrics Society found that 67% of older adults who had a double ingredient incident said their providers never asked about non-prescription drugs. That’s not negligence-it’s a system flaw. Doctors don’t have time to dig through every bottle. But you can fix that.How to Protect Yourself: 5 Simple Steps
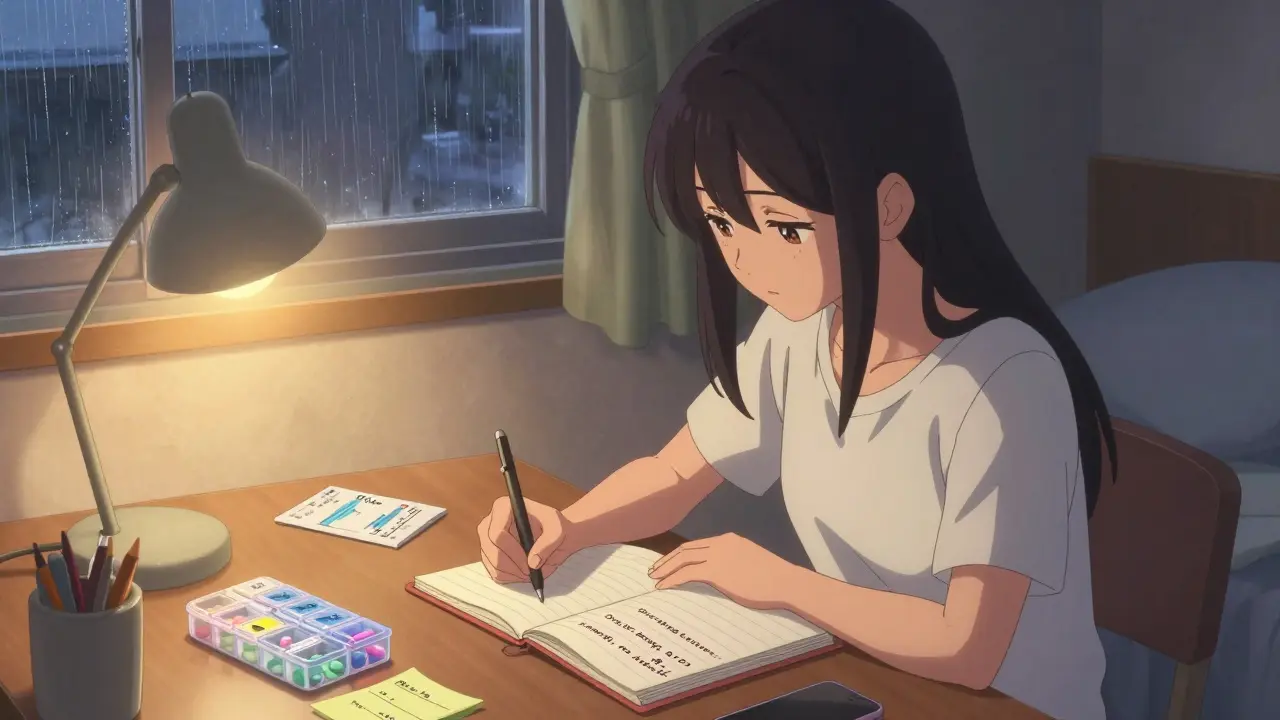
You don’t need a pharmacy degree to avoid double ingredients. Here’s what works:- Make a complete medication list. Write down every pill, liquid, patch, cream, and supplement you take-daily or occasionally. Include the name, dose, how often, and why you take it. Don’t forget OTC drugs, vitamins, and herbal teas. Keep a printed copy in your wallet and another at home.
- Use one pharmacy. Filling all your prescriptions at the same place cuts your risk of double ingredients by 63%. Pharmacists have systems that flag duplicates. If you use multiple pharmacies, they can’t see what the other one filled.
- Ask your pharmacist every time. When you pick up a new prescription or OTC product, say: “Could this interact with anything else I’m taking?” Pharmacists catch double ingredients in 87% of medication reviews. They’re trained for this. Use them.
- Review your meds once a year. Set a date-maybe your birthday or New Year’s Day-and sit down with your primary doctor. Bring your list. Ask: “Are all of these still necessary? Could any be duplicates?” A 2021 study showed this reduces errors by 54%.
- Check OTC labels like a detective. Before buying anything, look at the “Active Ingredients” section. Don’t just read the brand name. If you see acetaminophen, diphenhydramine, or ibuprofen, compare it to your list. If it’s already on there, don’t take it.
Technology Can Help-But Don’t Rely on It Alone
New tools are making it easier. Apple Health now flags duplicate ingredients in iOS 17. Apps like MedWise Risk Score analyze your meds and give you a risk score. Electronic health records from Epic and Cerner now alert doctors if you’re about to get a duplicate. But here’s the catch: these systems only work if your meds are entered correctly. If you didn’t tell your doctor you take melatonin every night, or if you refill your cold medicine at a different pharmacy, the system won’t know. Technology is a helper-not a safety net. Your list is your real shield.What to Do If You Think You’ve Taken Too Much
If you feel unusually sleepy, confused, nauseous, or have pain in your upper right abdomen (where your liver is), stop taking everything except water. Call your doctor or go to urgent care. Don’t wait. Acetaminophen overdose can cause silent liver damage. You might not feel sick until it’s too late. The sooner you get tested, the better your chances.Final Thought: You’re the Only One Who Can Prevent This
Doctors, pharmacists, and apps can help-but they can’t read your mind. Only you know what you’ve taken today, last week, or when you felt a little under the weather. Double ingredient errors are 89% preventable, according to the American Academy of Family Physicians. That means if you take one extra step-checking your list-you’re likely avoiding a trip to the ER. Start today. Grab a pen. Write down everything you take. Then, next time you walk into a pharmacy or doctor’s office, hand them that list. It’s the simplest, most powerful thing you can do to stay safe.Can I take two different brands of pain relievers if they have different names?
No. Brand names don’t matter-active ingredients do. For example, Tylenol, Excedrin, and many prescription painkillers all contain acetaminophen. Taking two together-even if they’re called different things-can cause an overdose. Always check the “Active Ingredients” section on the label.
I take a lot of supplements. Could those cause double ingredients?
Yes. Many supplements contain hidden active ingredients. For example, some sleep aids include melatonin and diphenhydramine. Others have herbal extracts like valerian root or kava, which can act like sedatives. If you’re also taking prescription sleep or anxiety meds, combining them can be dangerous. Always include supplements on your medication list.
Why don’t doctors always check for OTC meds?
Most doctors focus on treating one condition at a time and have limited time per visit. Many assume patients will mention OTC drugs, but patients often don’t realize they’re important. Studies show nearly 70% of older adults never volunteer this info. That’s why you need to bring your list-don’t wait for them to ask.
Is it safe to take OTC meds with my prescription if my doctor didn’t say no?
Not necessarily. Just because your doctor didn’t warn you doesn’t mean it’s safe. Many prescriptions don’t list all possible OTC interactions. And if your doctor didn’t know you were taking the OTC drug, they couldn’t warn you. Always check with your pharmacist before combining anything.
How often should I update my medication list?
Update it every time you start, stop, or change a dose-whether it’s a prescription, OTC, or supplement. At minimum, review it every 6 months. Keep the latest version with you at all times, especially if you have chronic conditions or take five or more medications.



Babe Addict
December 27, 2025 AT 06:16Look, I get it - acetaminophen is everywhere. But let’s be real, if you can’t read a drug label, maybe you shouldn’t be allowed to buy anything beyond toilet paper. I’ve seen people grab NyQuil and Tylenol like they’re candy. The real problem isn’t the meds - it’s the people who think ‘natural’ means ‘safe’ and take five herbal sleep powders on top of their prescriptions. Wake up. You’re not special. Your liver doesn’t care how ‘holistic’ you are.
Satyakki Bhattacharjee
December 28, 2025 AT 02:40Life is simple. Take one thing at a time. The body knows how to heal. Modern medicine is a temple of confusion. We have forgotten the old ways - rest, water, silence. Why do we need so many pills? Because we have lost our connection to nature. A man who eats real food and sleeps under the stars does not need NyQuil. He needs to breathe.
Kishor Raibole
December 29, 2025 AT 05:31It is with profound regret that I observe the alarming proliferation of polypharmacy in contemporary society - a phenomenon not merely medical, but sociocultural in its origins. The conflation of pharmaceutical convenience with therapeutic necessity has engendered a collective myopia wherein the individual relinquishes agency to the algorithmic dictates of corporate pharmacology. One must ask: Who benefits from the normalization of concurrent acetaminophen ingestion across six distinct proprietary formulations? The answer, regrettably, is not the patient.
John Barron
December 29, 2025 AT 07:24As a board-certified clinical pharmacologist with 22 years in the field, I can confirm: this is the #1 preventable cause of acute liver failure in middle-aged Americans. 🚨 And yes, I’ve seen patients die from this. Not because they were careless - because the system is designed to let them fail. The FDA’s ‘Drug Facts’ label? A joke. 41% can’t read it? That’s not ignorance - it’s negligence. I’ve trained 300+ residents. NONE of them were taught how to explain this to a 70-year-old with 12 prescriptions. 🤦♂️
Liz MENDOZA
December 29, 2025 AT 11:01I just wanted to say thank you for writing this. My mom almost ended up in the ER last year because she took her arthritis pill and a cold medicine that both had ibuprofen. She didn’t know - no one ever told her. I printed out a simple list for her, wrote the names in big letters, and now she carries it in her purse. It’s not glamorous, but it saved her. If you’re reading this and you take more than 3 meds - please, just write them down. You don’t need to be a doctor. You just need to care enough to try.
Anna Weitz
December 29, 2025 AT 17:28Why are we even surprised by this? The whole system is rigged. Big Pharma wants you confused. They put the same ingredient in 50 brands so you keep buying. They don’t want you to know what’s in your meds because then you’d stop trusting them. Doctors don’t care because they get paid per script. Pharmacists? They’re overworked and underpaid. You think they’re gonna check your 17 bottles? Nah. You’re on your own. Welcome to healthcare in America 🤷♀️
Jane Lucas
December 29, 2025 AT 20:44lol i just took tylenol and a cold med yesterday and now im paranoid 😅 but seriously i never check the active stuff. i just read the brand name and go. this is a wake up call. i’m making a list tonight
Caitlin Foster
December 31, 2025 AT 19:04OMG I JUST REALIZED I’VE BEEN TAKING DIPHENHYDRAMINE IN MY SLEEP PILLS AND MY ALLERGY MED FOR 3 YEARS 😱 I’M SO GLAD I READ THIS BEFORE I TURNED INTO A ZOMBIE. THANK YOU. I’M THROWING OUT MY UNISOM AND BUYING A NEW LIST. I’M TAKING THIS SERIOUSLY NOW 💪
Robyn Hays
January 1, 2026 AT 02:13This made me think about my grandma - she takes 8 things a day, and I swear half of them are ‘just in case.’ I started helping her organize her meds into a little box with labels, and now she says she feels more in control. It’s not about being perfect - it’s about being aware. If you’re taking anything, even a gummy vitamin, write it down. Even the ‘harmless’ ones. You never know what’s hiding in there. And hey - if you’re nervous about asking your doctor, just say: ‘I want to make sure I’m not doubling up.’ They’ll thank you for it.
Liz Tanner
January 2, 2026 AT 06:36One pharmacy. Always. I didn’t realize how much this mattered until my dad switched pharmacies and got a new prescription that had the same ingredient as his blood pressure med. He ended up with a nasty stomach bleed. Now we only use one pharmacy, and I print his list every time he sees a new doctor. Simple. Free. Life-saving. Why isn’t this taught in high school?
Elizabeth Alvarez
January 3, 2026 AT 20:27Let me tell you what’s really going on. The government, the FDA, the pharmaceutical giants - they’re all in cahoots. They want you dependent. They want you confused. Why? Because if you knew how many of these pills are just repackaged sugar with a patent, you’d revolt. The ‘active ingredients’ are designed to be invisible. The labels? Written in tiny font on purpose. The ‘56,000 ER visits’? That’s just the tip of the iceberg. They don’t count the ones who die quietly at home. They don’t count the ones who get misdiagnosed because their liver enzymes are off from acetaminophen overload. This isn’t an accident. It’s a controlled population management strategy. Wake up.
Miriam Piro
January 4, 2026 AT 11:12They’re watching you. Every time you buy a cold medicine, they track it. Every time you refill a prescription, it’s logged. The algorithm knows you’re taking 3 things with acetaminophen. But instead of warning you, they let you overdose - then sell you the liver transplant. 💀 I know this because I saw the whistleblower documents. The FDA has a hidden database of ‘high-risk polypharmacy patients.’ They don’t call you. They don’t email you. They just wait. And when you collapse, the insurance company gets paid. The system is designed to fail you. Don’t be a statistic. Burn your list. And then burn the system.
dean du plessis
January 5, 2026 AT 08:11Interesting post. I live in South Africa and here people use traditional herbs a lot - like muti for pain or sleep. Sometimes it has hidden stuff like caffeine or even steroids. I’ve seen people combine it with their blood pressure meds and end up in hospital. The real issue isn’t just the pills - it’s the lack of communication between modern and traditional healers. Maybe the solution is a simple app where you scan your bottle and it flags matches. But even better - just talk to someone. Ask. Even if it feels awkward.
Kylie Robson
January 7, 2026 AT 03:58Acetaminophen hepatotoxicity is the most common cause of acute liver failure in the U.S. and the UK, with a median dose of 7.5g in unintentional overdoses - well above the 4g/day threshold. The pharmacokinetics are nonlinear above 4g, meaning clearance drops sharply and NAPQI accumulation becomes exponential. This is why the FDA lowered the max daily dose to 3g for chronic users in 2011 - but most OTC labels still say 4g. Regulatory lag. Also, CYP2E1 polymorphisms affect metabolic susceptibility - some populations have higher risk. You need genetic screening for chronic users. But nobody does it. Because profit > safety.
John Barron
January 9, 2026 AT 00:44Just saw @6324’s comment about your mom. That’s exactly why I started teaching my patients to use a pill organizer with a printed list taped to the lid. I give them a free one at every visit. It’s not fancy, but it works. And if you’re a caregiver - do it for them. They’ll forget. That’s not their fault. It’s just how aging works. You’re not being overbearing - you’re being their safety net.