Nitrofurantoin and Hemolytic Anemia: What You Need to Know About G6PD Deficiency Risk

Nitrofurantoin Safety Checker
Personal Risk Assessment Tool
This tool helps you understand your individual risk of hemolytic anemia when taking nitrofurantoin based on key factors discussed in the article.
Your Risk Assessment
Every year, millions of people take nitrofurantoin to treat a simple urinary tract infection (UTI). It works fast, it’s cheap, and for most people, it’s safe. But for a significant number of others, this common antibiotic can trigger a life-threatening reaction they never saw coming: hemolytic anemia. And the biggest risk? Having undiagnosed G6PD deficiency.
What is nitrofurantoin, and why is it so commonly used?
Nitrofurantoin, sold under brand names like Macrobid and Furadantin, has been around since the 1940s. It’s not a flashy drug, but it’s effective. It targets bacteria in the urinary tract-especially E. coli, the usual culprit behind UTIs-and it does so in a way that makes resistance slower to develop than with other antibiotics like trimethoprim-sulfamethoxazole. That’s why doctors still reach for it. In the U.S. alone, about 5.5 million prescriptions are filled each year.
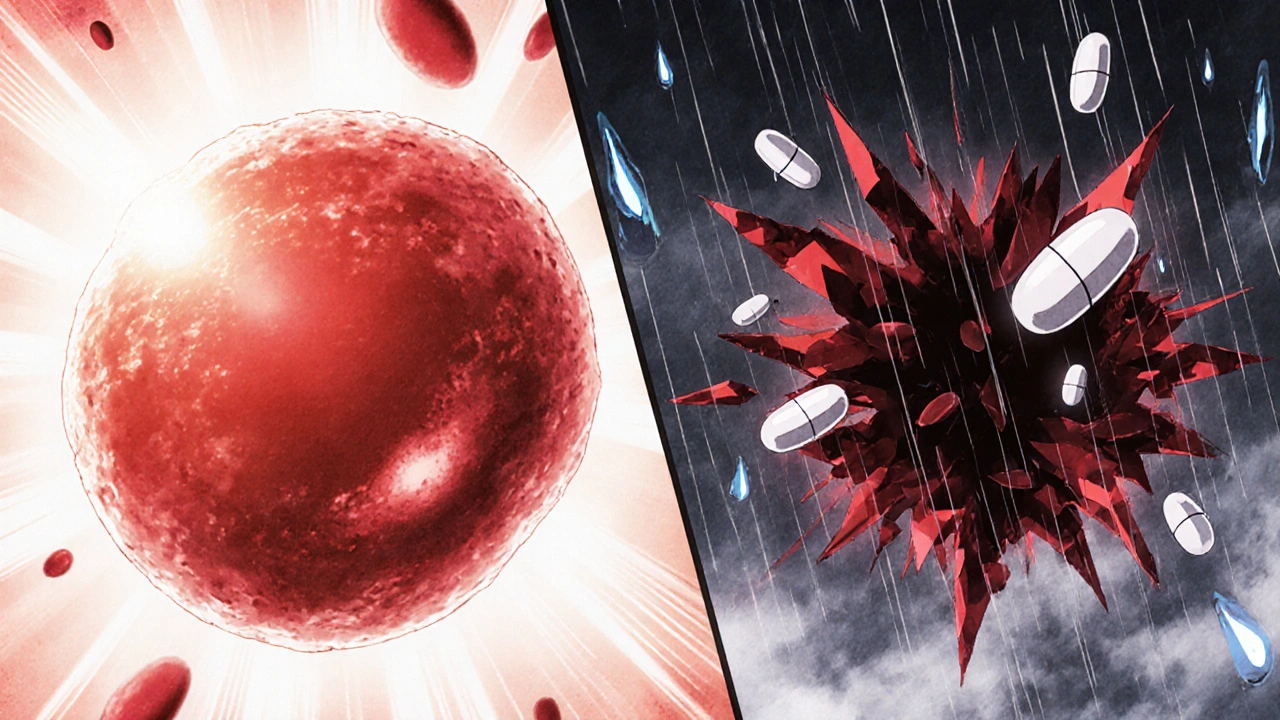
But here’s the catch: nitrofurantoin doesn’t just attack bacteria. It also creates oxidative stress in the body. For healthy people, that’s not a problem. Their red blood cells have enough defense mechanisms to handle it. But for people with G6PD deficiency, those defenses are broken.
What is G6PD deficiency, and why does it matter?
G6PD (glucose-6-phosphate dehydrogenase) deficiency is a genetic condition that affects how your red blood cells protect themselves from damage. It’s inherited, mostly passed down through the X chromosome, which is why it’s more common in men. But women can carry and pass it on too.
Worldwide, about 400 million people have this condition. It’s especially common in people of African, Mediterranean, Middle Eastern, and Southeast Asian descent. In Black African and African American populations, up to 14% may be affected. In Mediterranean regions, it’s around 5%. Many people don’t know they have it-until they take a drug like nitrofurantoin.
Without enough G6PD enzyme, red blood cells can’t make enough glutathione, the main antioxidant that keeps them stable. When nitrofurantoin enters the system, it floods the bloodstream with oxidizing agents. The red blood cells can’t fight back. They break apart. That’s hemolysis. And when enough red blood cells die off at once, you get hemolytic anemia.
How dangerous is nitrofurantoin for someone with G6PD deficiency?
It’s not just risky-it’s potentially deadly.
Studies have documented at least 42 confirmed cases of hemolytic anemia directly linked to nitrofurantoin in G6PD-deficient patients. Ten of those cases ended in death. Symptoms show up fast: fever, chills, dark urine, fatigue, jaundice, rapid heartbeat, and sometimes confusion or low blood pressure. Lab tests show plummeting hemoglobin, rising bilirubin, low haptoglobin, and high LDH-all signs your red blood cells are being destroyed.
One 2023 case report described a patient who started nitrofurantoin for a UTI. Within 48 hours, they were hospitalized with severe anemia. Their hemoglobin dropped from 13 g/dL to 7.2 g/dL. They didn’t need a blood transfusion, but they did need IV fluids and to stop the drug immediately. They recovered fully-but only because it was caught early.
The problem? Many doctors don’t screen for G6PD deficiency before prescribing nitrofurantoin. A 2022 survey of 350 primary care physicians found only 32% routinely check for it. That’s alarming. Especially when you consider that half to 60% of people with G6PD deficiency are undiagnosed until they have a reaction like this.
Who’s at highest risk?
It’s not just about ethnicity. Certain groups are more vulnerable:
- Pregnant women: Eight documented cases of hemolytic anemia occurred in pregnant women taking nitrofurantoin. The drug crosses the placenta. If the mother has G6PD deficiency-or the baby inherited it-the fetus is at risk too.
- Infants: Two cases were linked to maternal use during breastfeeding. One case was an overdose in a newborn.
- People with kidney problems: Nitrofurantoin is cleared by the kidneys. If kidney function is poor (eGFR under 60), the drug builds up in the blood, increasing the chance of toxicity-even in people without G6PD deficiency.
That’s why the FDA says nitrofurantoin shouldn’t be used in patients with moderate to severe kidney impairment. But many doctors still prescribe it without checking kidney function or G6PD status.
What do medical guidelines say?
The guidance is clear-but not always followed.
The American Society of Hematology says: “Nitrofurantoin should be avoided in patients with known G6PD deficiency.”
The Clinical Pharmacogenetics Implementation Consortium (CPIC) goes further. They classify nitrofurantoin as a drug that requires caution in G6PD-deficient patients without chronic hemolytic anemia-and complete avoidance in those who have it.
They’re not being overly cautious. They’re being realistic. The drug’s benefits don’t outweigh the risks for this group. And there are safer alternatives.
What are the safer alternatives for UTIs?
If you have G6PD deficiency-or you’re in a high-risk group-there are other options:
- Fosfomycin: A single-dose oral antibiotic. No known risk of hemolysis. Often used as first-line for uncomplicated UTIs in G6PD-deficient patients.
- Cephalexin: A cephalosporin with low oxidative risk. Used widely and generally safe.
- Pivmecillinam: Available in Europe and other regions. Low hemolytic risk.
- Trimethoprim-sulfamethoxazole (TMP-SMX): Higher resistance rates than nitrofurantoin, but still used. Avoid if you have a sulfa allergy.
For most people, fosfomycin is the best choice. It’s effective, single-dose, and doesn’t carry the oxidative burden of nitrofurantoin. The downside? It’s more expensive. But compared to the cost of a hospital stay for hemolytic anemia-$8,500 to $12,000-it’s a bargain.
Should everyone be tested for G6PD deficiency before taking nitrofurantoin?
Not necessarily. But you should be tested if you fit one of these profiles:
- You’re of African, Mediterranean, Middle Eastern, or Southeast Asian descent
- You have a family history of anemia or jaundice after taking certain drugs
- You’ve had unexplained anemia, dark urine, or jaundice in the past
- You’re pregnant and from a high-risk population
The test is simple: a blood test that costs between $35 and $50. It takes minutes to get results with point-of-care tests now available in some clinics. That’s less than the price of a coffee-and far cheaper than a trip to the ER.
Some hospitals and clinics are starting to build alerts into their electronic health record systems. If you’re flagged as high-risk, the system prompts the doctor to consider alternatives. But this isn’t universal yet.
What should you do if you’re prescribed nitrofurantoin?
Don’t panic. But don’t just take it without asking questions.
- Ask your doctor: “Do I have G6PD deficiency?”
- Ask: “Is there a safer antibiotic for me?”
- Ask: “Have you checked my kidney function?”
- If you’re from a high-risk ethnic group, insist on a G6PD test before filling the prescription.
If you start taking nitrofurantoin and feel worse within 2-3 days-fever, dark urine, extreme fatigue, yellowing skin-stop the drug and go to urgent care immediately. Hemolytic anemia from nitrofurantoin can be reversed if caught early. But waiting too long can lead to kidney failure, shock, or death.
The bigger picture: Why isn’t this better known?
Nitrofurantoin remains one of the top 5 antibiotics for UTIs in the U.S., even though its risks are well-documented for decades. The 1956 JAMA case report was the first to link it to hemolytic anemia. Since then, hundreds more have followed.
Regulators haven’t acted strongly enough. The FDA’s label warns about G6PD deficiency-but doesn’t require screening. The EMA updated its warning in 2021. But in many clinics, the conversation never happens.
Meanwhile, the global market for G6PD testing is expected to grow to $310 million by 2027. Why? Because more doctors are realizing that preventing one case of drug-induced hemolysis saves more money-and lives-than treating it.
Nitrofurantoin isn’t going away. It’s too useful for resistant infections. But its use needs to be smarter. For the millions who can safely take it, it’s a lifesaver. For those with G6PD deficiency, it’s a ticking time bomb. And too many people are still walking into that danger zone without knowing it.


gina rodriguez
November 29, 2025 AT 07:25Nitrofurantoin was prescribed to my mom last year for a UTI. She’s African American and had never been tested for G6PD. Thank god she noticed the dark urine and called the doctor right away. They stopped it, did the test, and confirmed the deficiency. She’s fine now, but it scared us both to death. Please, if you’re from a high-risk group, just ask for the test. It’s 50 bucks and could save your life.
Sue Barnes
November 29, 2025 AT 23:08Doctors are lazy. They don’t want to think, so they just prescribe the cheapest, most popular drug. Nitrofurantoin is a trap for people who look ‘healthy’ on paper. If you’re Black, Mediterranean, or Asian, you’re basically playing Russian roulette every time you get a UTI script. Someone needs to sue the AMA for this negligence.
jobin joshua
November 30, 2025 AT 20:37Brooooo, I had G6PD deficiency and didn’t know it 😱 My cousin died from this in India… I’m so glad I found out after my first bad reaction. Now I carry a medical card. Please, if you’re from South Asia, get tested. It’s like a free vaccine against death 💉❤️
Sachin Agnihotri
December 1, 2025 AT 19:42So many people don’t realize how common G6PD deficiency is… I’m from India, and in my family alone, three people have it. My uncle had a near-fatal reaction to sulfa drugs back in the 90s. Now we all get tested before any new meds. It’s not complicated. Just a finger prick. Why is this not standard? I mean… seriously?
Diana Askew
December 2, 2025 AT 23:32Big Pharma doesn't want you to know this. They profit off ER visits. G6PD testing? Too cheap. Nitrofurantoin? Billions in sales. The FDA is in their pocket. And they're letting people die so they can keep selling poison. You think this is an accident? It's a business model. 🕵️♀️💊
King Property
December 4, 2025 AT 10:23Let me school you. Nitrofurantoin has been flagged since 1956. The FDA label says it right there. If you didn’t read the label, that’s your fault. Also, fosfomycin isn’t always available. Sometimes nitrofurantoin is the ONLY option. Stop blaming doctors. Blame your ignorance. And stop acting like everyone’s a victim.
Pawittar Singh
December 5, 2025 AT 09:07Hey, I get it - you're scared. But here’s the good news: you can control this. 🙌 If you’re from a high-risk background, ask your doc for a quick G6PD test. It’s easy, fast, and cheap. I’ve helped three friends get tested after reading this. One saved their life. You don’t need to be a genius - just proactive. You got this 💪❤️
Josh Evans
December 5, 2025 AT 11:40My sister took nitrofurantoin and got jaundice. We thought it was just a virus. Turned out it was hemolysis. She was in the hospital for 3 days. We never even heard of G6PD before. Now we tell everyone. This info needs to be on every prescription bottle. Like, literally. ‘WARNING: MAY KILL YOU IF YOU HAVE G6PD DEFICIENCY’.
Allison Reed
December 6, 2025 AT 20:47This is exactly the kind of public health issue that flies under the radar because it affects marginalized populations. The fact that 60% of people with G6PD deficiency are undiagnosed isn’t a coincidence - it’s systemic neglect. Thank you for highlighting this. Let’s push for mandatory screening in high-risk groups before prescribing nitrofurantoin. It’s not radical. It’s responsible.
Jacob Keil
December 7, 2025 AT 08:28so like… life is just a series of chemical reactions right? and our bodies are just… fragile little machines? and drugs? they’re just… blunt instruments? and we’re all just… playing russian roulette with our red blood cells? 😭
Rosy Wilkens
December 8, 2025 AT 22:24This is why I never trust Western medicine. They don’t care about your ancestry. They don’t care about your heritage. They just push pills. I’m from a family where three people died from ‘unexplained jaundice’ after antibiotics. They called it ‘idiopathic’. It was G6PD. They buried the truth. This isn’t medicine. It’s cultural genocide.
Andrea Jones
December 10, 2025 AT 12:03Wait… so you’re telling me I could’ve died from a UTI antibiotic I got from CVS? 😳 And my doctor didn’t even blink? That’s… honestly kind of hilarious. In a ‘I’m about to cry’ way. I’m getting tested tomorrow. And I’m sending this to every woman I know. You’re welcome, universe.
Justina Maynard
December 10, 2025 AT 12:07Let’s be real - if this was a drug that only affected white people, there’d be a congressional hearing, a Netflix docu-series, and a celebrity PSA with Meryl Streep crying on a podium. But since it’s mostly people of color? We get a footnote in a 12-page PDF no one reads. The system is rigged. And I’m done pretending it’s not.