Biosimilars vs Generics: What You Need to Know About the Key Differences

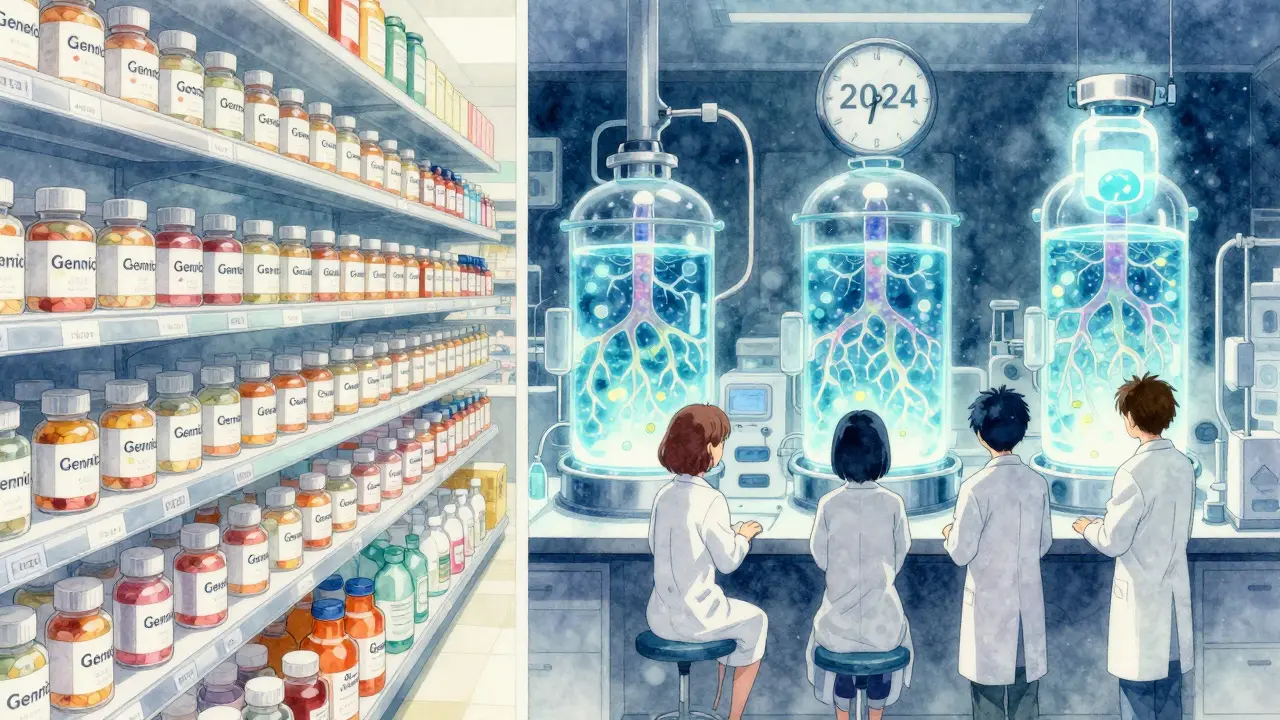
When you hear "generic drug," you probably think of a cheaper version of your prescription-same pill, same effect, lower price. But what about biosimilars? They’re also cheaper alternatives to expensive brand-name drugs, but they’re not the same as generics. Confusing them is common-and it can lead to misunderstandings about safety, cost, and how they work in your body.
What Are Generics, Really?
Generics are exact chemical copies of brand-name drugs. Take ibuprofen, for example. The brand version is Advil. The generic is just ibuprofen. Same active ingredient. Same dosage. Same way your body absorbs it. The FDA requires generics to be bioequivalent-meaning they deliver the same amount of medicine into your bloodstream at the same rate as the original. That’s why pharmacists can swap them out without asking your doctor.Generics are made from simple, synthetic chemicals. Their structure is tiny-like aspirin, which weighs about 180 daltons. Because they’re so small and straightforward, manufacturers can reproduce them exactly. That’s why there are over 10,000 generic drugs on the market in the U.S., making up 90% of all prescriptions filled. And they save you money: typically 40% to 50% less than the brand name.
What Are Biosimilars?
Biosimilars are different. They’re not copies. They’re highly similar versions of biologic drugs-medicines made from living cells, not chemicals. Think of them like a handcrafted wooden chair that looks and functions almost exactly like the original, but was made by a different carpenter using slightly different tools. The result? Nearly identical, but not perfectly the same.Biologics are huge molecules-up to 5,000 times larger than small-molecule drugs. For example, infliximab (Remicade) weighs about 148,000 daltons. These drugs are made using living cells-bacteria, yeast, or animal cells grown in labs. Tiny changes in temperature, pH, or nutrients during production can affect the final product. That’s why biosimilars can’t be exact copies. But they must be so close that there’s no meaningful difference in safety or effectiveness, according to the FDA.
As of November 2023, the FDA has approved 42 biosimilars. Most target high-cost treatments for cancer, autoimmune diseases like rheumatoid arthritis, and diabetes. They’re not new drugs-they’re follow-ons to expensive biologics like Humira, Enbrel, and Herceptin.
The Regulatory Divide
The rules for getting generics and biosimilars approved couldn’t be more different.For generics, the path is simple: prove bioequivalence. That usually means running a few tests showing your version gets absorbed into the blood the same way as the brand. No need for big clinical trials. The process costs around $2 million to $5 million.
Biosimilars? It’s a whole different ballgame. Manufacturers must prove similarity through hundreds of lab tests-analyzing protein structure, function, purity, and stability. They need animal studies. Sometimes, clinical trials. And they can’t use the original manufacturer’s recipe. They have to reverse-engineer it. That’s why developing a biosimilar costs $100 million to $200 million.
The FDA’s approval process for biosimilars is governed by the Biologics Price Competition and Innovation Act (BPCIA) of 2009. Generics follow the Hatch-Waxman Act from 1984. Different laws. Different standards. Different complexity.

Can You Swap Them at the Pharmacy?
This is where it gets tricky.With generics, substitution is automatic. In every state, a pharmacist can give you the generic version without checking with your doctor. It’s built into the system.
With biosimilars, it’s not that simple. Only biosimilars labeled as "interchangeable" can be swapped without a doctor’s approval. And as of 2023, only 7 out of the 42 approved biosimilars have that status. That means most of the time, your doctor has to specifically prescribe the biosimilar. Even if it’s cheaper, the pharmacy can’t switch it on their own.
Why the restriction? Because biologics can trigger immune reactions. If you’re stable on Humira and your pharmacist swaps you for a biosimilar without your doctor knowing, there’s a small risk your body could react differently. That’s why experts like the American Society of Health-System Pharmacists say biosimilars aren’t automatically substitutable.
Cost Savings: Generics vs Biosimilars
Generics save you a lot. Biosimilars save you less.Generics typically cost 40% to 50% less than the brand-name version. A month’s supply of generic lisinopril might be $5. The brand? $50.
Biosimilars? They save 15% to 33%-sometimes up to a third less than the original biologic. That’s still significant, especially for drugs that cost $10,000 a month. But it’s not the same as the 90% discount you get with generics.
Why the gap? Manufacturing complexity. Biologics are hard to make. Even if you’ve got the formula, replicating it with living cells is unpredictable. That drives up costs-and limits how low prices can go.
Who Uses Them and Why?
Generics are everywhere. You’ve probably taken one without realizing it. They’re used for blood pressure, cholesterol, antibiotics, pain relievers-basically every common condition.Biosimilars are focused on specialty care. They’re mostly used in oncology, rheumatology, and endocrinology. For example, biosimilars for trastuzumab (Herceptin) are helping cancer patients afford treatment. Biosimilars for adalimumab (Humira) are changing how people with psoriasis and Crohn’s disease manage their condition.
Hospitals and specialty pharmacies are leading the way in adopting biosimilars. About 45% of U.S. hospitals now use at least one biosimilar. But primary care doctors? Many still don’t feel confident prescribing them. A 2022 survey found 68% of rheumatologists wanted more training before switching patients.
What Experts Say
There’s a clear consensus: biosimilars are not generics.Dr. Gary Gibbons from the National Heart, Lung, and Blood Institute put it plainly: "Biosimilars require a fundamentally different regulatory approach than generics." The FDA echoes this. Their educational materials say: "Biosimilars are not generics-and important differences exist between them."
Dr. Rachel B. Ballow, a pharmaceutical scientist, explains it simply: "Because each reference product’s manufacturing process is proprietary information, the manufacturer’s biosimilar product always differs slightly from the reference product. This is in contrast to generic medications, which are identical to brand medications."
Some critics argue the savings aren’t worth the complexity. Dr. Paul Knoepfler points out that while generics save 40-50% with minimal risk, biosimilars offer only 15-20% savings-and require more monitoring. But others counter that for drugs costing $100,000 a year, even 20% is life-changing.
What’s Next?
The biosimilars market is growing fast. It was worth $10.3 billion in 2022 and could hit $37.2 billion by 2028. That’s a 23.8% annual growth rate. Meanwhile, generics are growing slowly-around 4% a year-because they’re already everywhere.Big changes are coming. The Inflation Reduction Act of 2022 is cutting out-of-pocket costs for Medicare patients on biologics. That’s pushing more insurers to favor biosimilars. In January 2024, the first interchangeable biosimilar for Humira hit the market with a 35% price cut. More are on the way.
Still, barriers remain. Drugmakers like AbbVie have used patent thickets-filing hundreds of patents-to delay biosimilar competition. It took until 2023 for Humira biosimilars to become widely available, even though the first was approved in 2016.
Future developments include "bio-super-similars"-biosimilars with improved properties-and clearer FDA guidance on interchangeability for complex biologics like antibody-drug conjugates.
Bottom Line
If you’re taking a pill you can buy over the counter, it’s probably a generic. Simple, safe, cheap.If you’re getting an injection for arthritis, cancer, or diabetes, it might be a biologic-and a biosimilar could be an option. It’s not a copy. It’s a close match. And while it won’t save you as much as a generic, it still cuts costs significantly.
Don’t assume they’re the same. Don’t assume you can swap them. Talk to your doctor. Ask if a biosimilar is right for you. And if you’re switching from a brand-name biologic, make sure your provider monitors you closely.
Both generics and biosimilars help make medicine more affordable. But they’re not interchangeable. Understanding the difference isn’t just academic-it can affect your treatment, your costs, and your health.
Are biosimilars the same as generics?
No. Generics are exact chemical copies of small-molecule drugs. Biosimilars are highly similar but not identical versions of complex biologic drugs made from living cells. They’re not interchangeable without special FDA approval.
Can pharmacists substitute biosimilars like they do with generics?
Only if the biosimilar has been designated as "interchangeable" by the FDA. As of 2023, only 7 out of 42 approved biosimilars have that status. For the rest, your doctor must specifically prescribe the biosimilar. Pharmacists can’t swap them automatically.
Why are biosimilars more expensive to develop than generics?
Biosimilars are made from living cells, which makes their structure far more complex than small-molecule generics. Manufacturers must replicate the original using their own methods, run hundreds of lab tests, and often conduct clinical trials. This costs $100-200 million. Generics cost $2-5 million because they’re chemically identical and easier to produce.
Do biosimilars work as well as the original biologics?
Yes. The FDA requires biosimilars to show no clinically meaningful differences in safety, purity, or potency compared to the original. Thousands of patients have used them safely. But because they’re not exact copies, switching from a brand-name biologic to a biosimilar should be done carefully and under medical supervision.
Why aren’t there more biosimilars in the U.S. than in Europe?
Europe adopted biosimilars faster due to stronger price pressure and clearer substitution rules. In the U.S., patent thickets, reimbursement models like "buy-and-bill," and provider hesitancy slowed adoption. As of 2023, biosimilars made up less than 3% of the U.S. biologics market, compared to 35% in Europe.
Is it safe to switch from a brand-name biologic to a biosimilar?
For most patients, yes-especially when initiated by a doctor. But switching between different biosimilars or back to the original brand should be done cautiously. The American College of Rheumatology recommends monitoring for immune reactions, especially in autoimmune conditions. Always discuss switching with your provider.


Angela Goree
January 3, 2026 AT 00:14Wow. Just... wow. This is why America’s healthcare system is a circus: we can make a pill that’s chemically identical for $5, but a protein made by yeast cells? Oh no, now it’s ‘complex’ and costs $10K. Let me guess-pharma’s patent lawyers wrote this article.
erica yabut
January 4, 2026 AT 06:42Oh honey, let’s not pretend biosimilars are some revolutionary breakthrough. They’re just Big Pharma’s cleverly disguised ‘me-too’ drugs with a fancy label and a 20% discount. Meanwhile, generics-real generics-have been saving lives for decades without the theatrics. If you need a biologic, fine. But don’t dress up a slightly different protein as ‘science.’ It’s marketing dressed in a lab coat.
Lori Jackson
January 5, 2026 AT 16:31Can we talk about how dangerous this is? Patients are being shuffled between biosimilars like they’re playing musical chairs with their immune systems. And the FDA? They’re acting like it’s just a different flavor of soda. No. This isn’t about cost. It’s about the sanctity of biological identity. If your body reacts differently because a protein folded slightly wrong? That’s not ‘no clinically meaningful difference.’ That’s a ticking time bomb. And someone’s making money off it.
Wren Hamley
January 7, 2026 AT 01:21So generics are like photocopying a crayon drawing. Biosimilars? That’s trying to paint the same Van Gogh using a different brush, different paint, and a slightly crooked canvas. You get the same vibe, same emotion-but if you’re an art critic, you’ll spot the brushstrokes. And yeah, it costs a fortune. But hey-at least it’s not a fake. It’s just… a very expensive homage.
Sarah Little
January 7, 2026 AT 03:38Interesting. But I’m curious-how many of these biosimilars have real-world pharmacovigilance data beyond clinical trials? I’ve seen patients on Humira switch to a biosimilar and develop neutralizing antibodies within 3 months. No one talks about that.
Hank Pannell
January 7, 2026 AT 04:59There’s an epistemological chasm here. Generics are ontologically identical; biosimilars are epistemologically similar. The former is a reductionist triumph of chemistry; the latter, a triumph of systems biology. We’re not just talking about molecular weight-we’re talking about emergent properties, post-translational modifications, glycosylation patterns. The FDA’s ‘no clinically meaningful difference’ is a statistical mirage. It’s not that biosimilars are unsafe-it’s that we don’t yet have the tools to measure the full spectrum of biological variability across populations. That’s the real frontier.
Palesa Makuru
January 8, 2026 AT 21:39Y’all in the US act like biosimilars are some alien technology. In South Africa, we’ve been using them for years because we can’t afford the original biologics. My cousin with rheumatoid arthritis? She’s on a biosimilar. Still walks. Still works. Still alive. You think because it’s not made in a lab in New Jersey, it’s less real? Please. The science is the same. The fear? That’s just privilege talking.
innocent massawe
January 10, 2026 AT 07:55Wow. This made me think. 😊 In Nigeria, we don’t even have generics for many drugs, let alone biosimilars. But I’m glad someone’s explaining it clearly. Maybe one day we’ll get these options too. Not everyone needs to save 50%-sometimes saving 20% means the difference between medicine and nothing. Thank you for this.
veronica guillen giles
January 10, 2026 AT 16:34Oh sweetie, you really think the average patient knows the difference between a generic and a biosimilar? No. They just see ‘cheaper’ and sign the form. Meanwhile, the pharmacy tech who swaps them doesn’t know the difference either. So who’s really protecting the patient? Not the system. Not the doctors. Definitely not the ads. It’s a beautiful, terrifying mess.
Philip Leth
January 10, 2026 AT 23:38My abuela takes generic metformin. Costs $4. My cousin with Crohn’s takes Humira. Costs $6K. Now there’s a biosimilar for $4K. She’s thrilled. She doesn’t care if it’s made by yeast or robots. She cares that she can eat without pain. Stop overcomplicating it. If it works, let people use it.
Ian Ring
January 11, 2026 AT 00:55Just one sentence: Biosimilars aren’t generics. And if you’re treating them like they are, you’re not just ignorant-you’re risking lives.