Prior Authorization Biosimilars: What You Need to Know Before Getting Covered
When your doctor prescribes a prior authorization, a process where your insurance company requires approval before covering a medication. It’s not a delay tactic—it’s a cost-control step built into most health plans. But when it comes to biosimilars, highly similar versions of complex biologic drugs that cost significantly less than the original, the rules get messy. Even though biosimilars are proven safe and effective, insurers often treat them like new drugs, forcing patients through extra hoops before they can get them.
Why? Because biologics—like Humira or Enbrel—are expensive, and insurers want to make sure you’ve tried cheaper alternatives first. That’s where prior authorization kicks in. But here’s the catch: many patients don’t realize biosimilars are not generics. They’re not pills you can swap out like aspirin. These are large, complex molecules made from living cells, so even small changes in production can affect how they work. That’s why insurers demand proof that switching won’t harm you. And yes, they often require you to fail on the original biologic first—even if your doctor says it’s not safe or effective for you.
Some states have passed laws to limit these delays, especially for autoimmune conditions like rheumatoid arthritis or Crohn’s disease. But nationally, the system is still patchy. If you’re prescribed a biosimilar, don’t assume it’s automatic. Call your pharmacy. Ask if prior authorization is needed. Check your insurer’s website for their step therapy list. And if your claim gets denied, know that appeals work—many are approved on the second try, especially with your doctor’s letter.
What you’ll find in these posts isn’t just theory. Real stories from people who fought insurance denials. Guides on how to talk to your pharmacist about biosimilar coverage. And breakdowns of which drugs trigger the most prior authorization headaches. You’ll also see how drug pricing, generic competition, and even patient education all tie into whether you get your medicine on time—or wait weeks for approval.
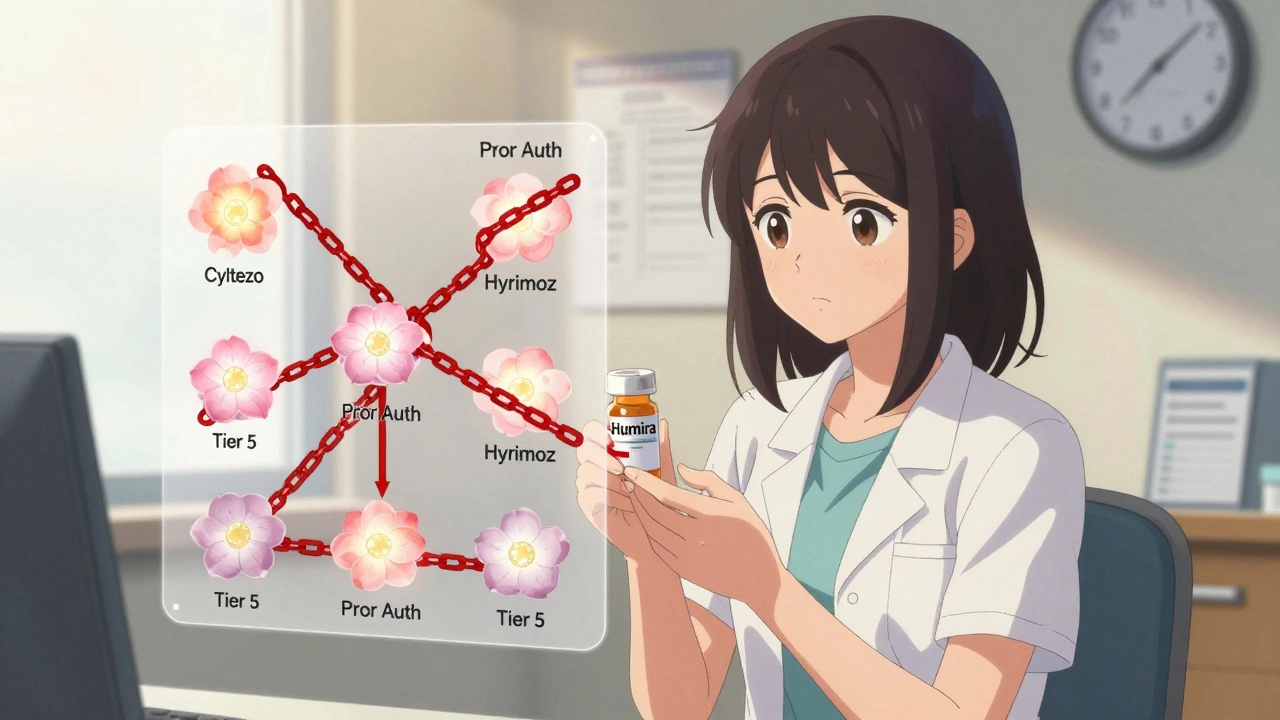
Insurance Coverage of Biosimilars: How Prior Authorization and Tier Placement Block Savings
Despite FDA approval of over 70 biosimilars, most insurance plans still treat them the same as expensive biologics like Humira-same tier, same prior authorization. This blocks savings and delays patient access.
VIEW MORE