Compare Antidepressants
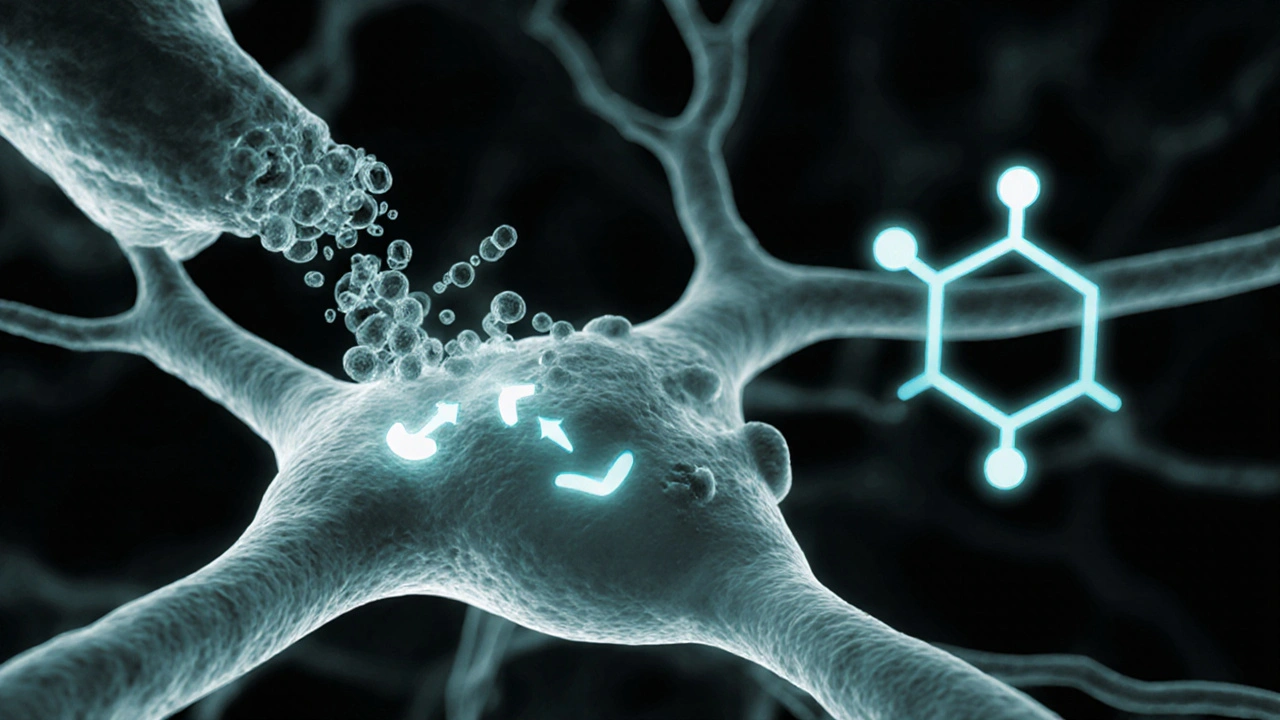
When you compare antidepressants, you’re evaluating how different mood‑lifting drugs perform in terms of efficacy, safety, cost, and patient preference. Also known as antidepressant comparison, it’s the process clinicians, patients, and caregivers use to match a drug to a specific case. This task brings together several key entities: SSRIs, selective serotonin reuptake inhibitors that boost serotonin levels, SNRIs, drugs that increase both serotonin and norepinephrine, tricyclic antidepressants, older agents that affect multiple neurotransmitters, and the condition itself, depression, a mood disorder characterized by persistent sadness and loss of interest. Comparing these pieces of the puzzle means looking at three semantic triples: "Antidepressant comparison assesses efficacy", "Side‑effect profile influences treatment choice", and "Cost considerations affect accessibility".
Key Factors When You compare antidepressants
First, efficacy isn’t a one‑size‑fits‑all number. Clinical trials report remission rates for SSRIs around 60‑70 %, while SNRIs often show a modest edge in severe cases. Tricyclics can be highly effective but carry a higher burden of cardiac and anticholinergic side effects. The second factor—side‑effect profile—directly shapes adherence. A patient prone to sexual dysfunction may favor an SNRI over certain SSRIs, whereas someone with insomnia might benefit from a mildly sedating tricyclic. Third, dosage flexibility matters; many SSRIs start at low doses and titrate up, while SNRIs have a narrower therapeutic window. Finally, cost and insurance coverage frequently tip the balance, especially for generic versions that make SSRIs a budget‑friendly pick.
Second, the severity and type of depression guide the class selection. Mild to moderate episodes often respond well to SSRIs, the go‑to first‑line option. When symptoms include significant fatigue or pain, SNRIs may provide added relief thanks to norepinephrine boost. For treatment‑resistant depression, clinicians sometimes revisit tricyclics or add augmentation agents. This relationship—"Depression severity determines antidepressant class"—creates a clear decision pathway and helps avoid trial‑and‑error prescribing.
Third, drug interactions and patient comorbidities are non‑negotiable considerations. SSRIs can inhibit CYP2D6, affecting medications like beta‑blockers, while SNRIs may raise blood pressure in hypertensive patients. Tricyclics require caution in people with heart disease due to QT prolongation risk. By mapping these interaction webs, you create a safer, more personalized comparison that respects the whole health picture.
Lastly, real‑world factors such as patient preference, formulation (tablet vs. liquid), and lifestyle play a role. Some people value a once‑daily dose, making certain SSRIs attractive. Others appreciate the flexibility of a split‑dose SNRI schedule to manage side effects throughout the day. Understanding these nuances turns a sterile table of numbers into a practical guide you can actually use.
Below you’ll find a curated collection of articles that dive deep into each of these areas—class‑by‑class breakdowns, side‑effect management tips, cost‑saving strategies, and step‑by‑step comparison charts. Use them to build your own comparison framework and choose the antidepressant that fits your unique needs.
Amitriptyline (Elavil) vs Top Alternatives: Benefits, Risks, and Best Uses
A clear, side‑by‑side comparison of Amitriptyline (Elavil) and its most common alternatives, covering uses, effectiveness, side effects, and how to choose the right option.
VIEW MORE