Amitriptyline (Elavil) vs Top Alternatives: Benefits, Risks, and Best Uses
Medication Selection Tool for Depression and Pain
Find the Best Medication for Your Needs
Answer a few questions about your symptoms and health profile to get personalized recommendations based on the latest clinical evidence.
When choosing a medication for depression or chronic nerve pain, many patients wonder how Amitriptyline (Elavil) measures up against newer options. This guide breaks down the science, side‑effect profiles, and real‑world suitability of Amitriptyline and its most common alternatives, so you can decide which drug-or non‑drug approach-fits your situation best.
What is Amitriptyline and How Does It Work?
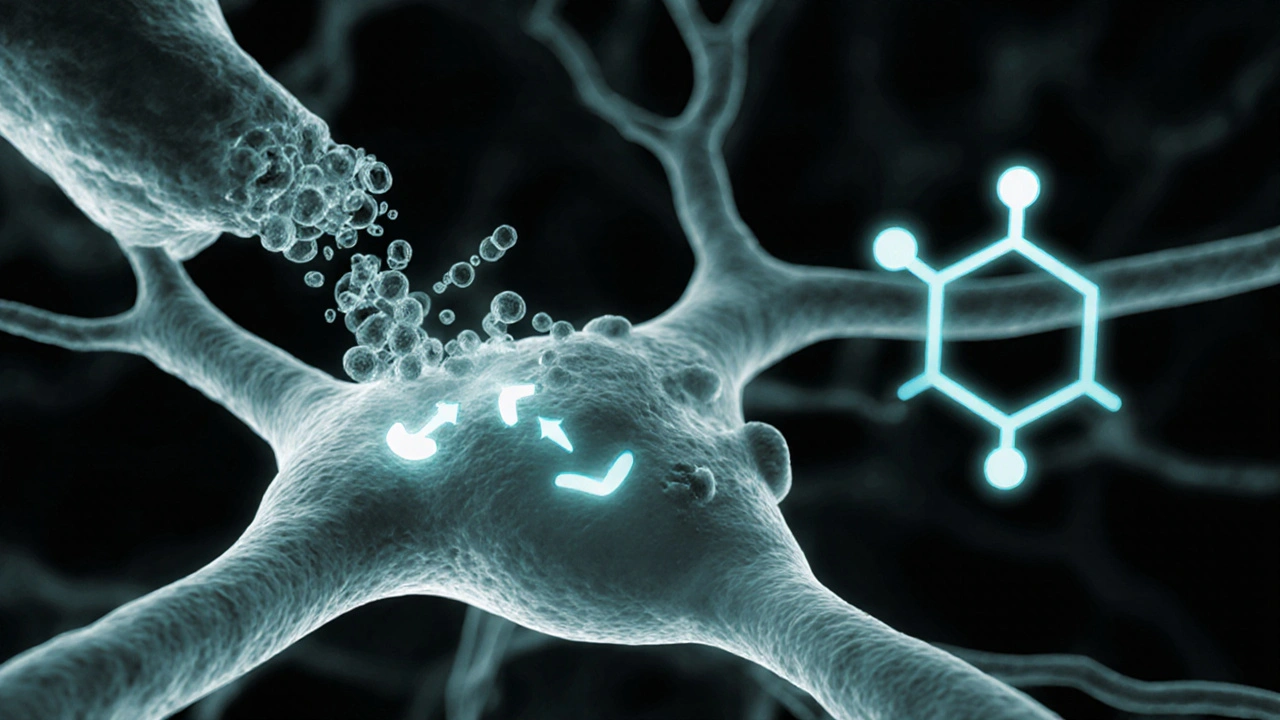
Amitriptyline is a tricyclic antidepressant (TCA) that blocks the reuptake of serotonin and norepinephrine, increasing their levels in the brain. It also has strong antihistamine and anticholinergic effects, which is why it can cause drowsiness and dry mouth. Traditionally prescribed for major depressive disorder, it’s also widely used off‑label for neuropathic pain, migraine prevention, and restless‑leg syndrome.
Key Alternative Classes
Over the past two decades, several drug classes have emerged that target the same neurotransmitters with fewer side effects. Below are the most relevant alternatives.
- Fluoxetine (Prozac) - a selective serotonin reuptake inhibitor (SSRI) first approved in 1987.
- Sertraline (Zoloft) - another SSRI with a slightly broader indication list.
- Venlafaxine (Effexor) - a serotonin‑norepinephrine reuptake inhibitor (SNRI) that bridges the gap between SSRIs and TCAs.
- Duloxetine (Cymbalta) - an SNRI approved for both depression and chronic musculoskeletal pain.
- Nortriptyline (Pamelor) - a TCA closely related to Amitriptyline but with fewer antihistamine effects.
- Mirtazapine (Remeron) - a noradrenergic and specific serotonergic antidepressant (NaSSA) that can boost appetite and sleep.
- Cognitive Behavioral Therapy (CBT) - a structured psychotherapy shown to be as effective as medication for mild‑to‑moderate depression.
Side‑Effect Landscape: Amitriptyline vs Alternatives
Understanding side‑effect profiles is crucial because they often dictate adherence.
| Medication | Common Side Effects | Serious Risks |
|---|---|---|
| Amitriptyline | Drowsiness, dry mouth, constipation, weight gain | Cardiac conduction delays, overdose toxicity |
| Fluoxetine | Insomnia, nausea, anxiety, sexual dysfunction | Serotonin syndrome, suicidal thoughts in young adults |
| Sertraline | Diarrhea, dizziness, sexual dysfunction | Serotonin syndrome, hyponatremia (rare) |
| Venlafaxine | Elevated blood pressure, nausea, sweating | Discontinuation syndrome, serotonin syndrome |
| Duloxetine | Dry mouth, fatigue, liver enzyme elevation | Hepatotoxicity, increased blood pressure |
| Nortriptyline | Less drowsiness than Amitriptyline, dry mouth | Cardiac effects (lower than Amitriptyline) |
| Mirtazapine | Weight gain, sedation, increased appetite | Rare agranulocytosis, metabolic syndrome |
Effectiveness for Depression and Pain
Clinical data show that Amitriptyline remains a solid first‑line option for neuropathic pain, often outperforming SSRIs in that niche. For pure depressive episodes, newer SSRIs and SNRIs tend to provide comparable mood improvement with a cleaner side‑effect slate.
| Condition | Amitriptyline | SSRIs (e.g., Fluoxetine) | SNRIs (e.g., Duloxetine) |
|---|---|---|---|
| Major Depressive Disorder | Response rate ~65% | Response rate ~68% | Response rate ~70% |
| Diabetic Neuropathic Pain | Pain reduction ~40% (NNT=3) | Minimal impact | Modest reduction ~25% (NNT=5) |
| Migraine Prophylaxis | Frequency drop ~50% | Not indicated | ~30% drop (some off‑label use) |
These numbers illustrate why clinicians often keep Amitriptyline in their toolbox for pain‑heavy patients, while reserving SSRIs/SNRIs for mood‑focused treatment.
Choosing the Right Medication: Decision Criteria
- Primary symptom focus - Is pain the dominant issue? Amitriptyline or Nortriptyline may win.
- Side‑effect tolerance - If drowsiness would impair work or driving, an SSRI like Fluoxetine might be safer.
- Cardiac health - Patients with arrhythmias should avoid TCAs; opt for Venlafaxine or Sertraline.
- Age and suicide risk - Young adults (<25) have higher SSRI‑related suicidal thoughts; a TCA might be considered only under close monitoring.
- Metabolic considerations - If weight gain is a concern, avoid Mirtazapine and Amitriptyline, lean toward Sertraline.
- Drug interactions - Amitriptyline inhibits CYP2D6, potentially raising levels of beta‑blockers, antipsychotics, and certain opioids.
Run through this checklist with your prescriber to pinpoint the safest, most effective match.
Practical Tips for Switching from Amitriptyline
- Gradually taper 10‑25mg every 3‑5days to reduce discontinuation syndrome.
- Start the new medication at a low dose (e.g., Fluoxetine 10mg daily) and titrate over 2‑4weeks.
- Maintain a symptom diary - note mood, pain, sleep, and any new side effects.
- Schedule a follow‑up visit within 2weeks of the switch to adjust dosage.
Quick Comparison Cheat‑Sheet
| Drug | Class | Typical Use | Starting Dose | Key Advantage | Key Drawback |
|---|---|---|---|---|---|
| Amitriptyline | Tricyclic | Depression, neuropathic pain | 10‑25mg HS | Strong analgesic effect | Sedation, cardiac risk |
| Fluoxetine | SSRI | Depression, OCD | 20mg daily | Long half‑life = easier taper | Insomnia, sexual side effects |
| Sertraline | SSRI | Depression, anxiety | 25mg daily | Well‑tolerated, low weight gain | Possible GI upset |
| Venlafaxine | SNRI | Depression, neuropathic pain | 37.5mg daily | Dual neurotransmitter action | Blood pressure rise |
| Duloxetine | SNRI | Depression, musculoskeletal pain | 30mg daily | FDA‑approved for pain | Liver monitoring needed |
| Nortriptyline | Tricyclic | Depression, migraine prophylaxis | 25mg daily | Fewer anticholinergic effects | Still carries cardiac caution |
| Mirtazapine | NaSSA | Depression with insomnia | 15mg HS | Improves sleep & appetite | Weight gain, sedation |
| Cognitive Behavioral Therapy | Psychotherapy | Mild‑moderate depression | - | No drug side effects | Requires therapist time, slower onset |

When Amitriptyline Might Still Be the Best Choice
If you suffer from chronic neuropathic pain that hasn’t responded to SSRIs or SNRIs, or if you need an inexpensive, off‑label option for migraine prevention, Amitriptyline often remains the most cost‑effective solution. Its broad receptor footprint can also help patients with co‑existing insomnia or anxiety, provided they can handle the sedating side effects.
Bottom Line Checklist
- Primary issue - pain?Amitriptyline or Nortriptyline.
- Need high alertness - consider an SSRI/SNRI.
- History of heart disease - avoid TCAs.
- Concern about weight gain - steer clear of Mirtazapine.
- Preference for non‑drug therapy - explore CBT.
Frequently Asked Questions
What conditions is Amitriptyline approved for?
Amitriptyline is FDA‑approved for major depressive disorder. It is also widely prescribed off‑label for neuropathic pain, migraine prophylaxis, and restless‑leg syndrome.
How does Amitriptyline compare to SSRIs for depression?
Both classes achieve similar remission rates (≈65‑70%). SSRIs typically cause less sedation and have a better cardiac safety profile, while Amitriptyline may be chosen if a patient also needs pain relief.
Is Amitriptyline safe for older adults?
Caution is advised. Older adults have higher risk of anticholinergic side effects (dry mouth, confusion) and cardiac conduction delays. Starting at 10mg and monitoring heart rhythm is standard practice.
Can I switch from Amitriptyline to an SNRI without a washout period?
Generally you can taper Amitriptyline over 1‑2weeks while introducing the SNRI at a low dose. Because Amitriptyline has a short half‑life, a strict washout isn’t required, but close supervision helps avoid serotonin syndrome.
What non‑drug options can replace Amitriptyline for chronic pain?
Consider SNRIs like Duloxetine (FDA‑approved for diabetic neuropathy), gabapentinoids, topical lidocaine patches, or structured physical therapy programs. Many patients combine a low‑dose TCA with these modalities for additive benefit.

Jessica Di Giannantonio
October 15, 2025 AT 20:08Wow, this rundown really shines a light on how versatile Amitriptyline can be! It's like a chameleon in the pharmacy world – stepping in for pain, insomnia, even restless‑leg syndrome when the newer kids shy away. I love that the guide breaks down the side‑effects so clearly; it makes the decision feel less like a gamble and more like a confident choice. If you’re battling nerve pain, the evidence here shows Amitriptyline still holds gold status, especially when the alternatives just nibble at the symptoms. Keep the optimism alive, folks, there’s still a place for the classics!
RUCHIKA SHAH
October 25, 2025 AT 20:08Amitriptyline works well for pain but can make you sleepy and thirsty. Newer drugs are lighter on the body but may not hit the nerve pain as hard. Choose what fits your daily life.
Justin Channell
November 4, 2025 AT 19:08Great summary! 👍 If you’re looking for a mood boost without the heavy drowsiness, SSRIs like Fluoxetine can be a smoother ride. But don’t forget Amitriptyline’s edge on neuropathic pain – sometimes the older meds keep the night pain at bay. 🌙 Stay hopeful and talk to your doc about what matters most for you.
Basu Dev
November 14, 2025 AT 19:08When we examine Amitriptyline in the broader context of antidepressant pharmacotherapy, several nuanced considerations emerge that merit thorough discussion. First, the pharmacodynamic profile of Amitriptyline, as a tricyclic agent, engages not only serotonin and norepinephrine reuptake inhibition but also antagonizes histamine H1 receptors and muscarinic cholinergic sites, which together underlie both its therapeutic versatility and its pronounced anticholinergic side‑effect burden. Second, the pharmacokinetic variability, especially concerning CYP2D6 metabolism, can lead to substantial inter‑patient differences in plasma concentrations, thereby influencing efficacy and toxicity risk. Third, the cardiac safety profile must be carefully weighed; TCAs, including Amitriptyline, can prolong QRS duration, a factor particularly relevant in patients with pre‑existing conduction abnormalities or those on concomitant QT‑prolonging agents. Fourth, comparative data consistently demonstrate that while SSRIs such as Fluoxetine and Sertraline provide comparable antidepressant response rates, they lack the robust analgesic efficacy observed with Amitriptyline in diabetic neuropathy, a distinction that becomes clinically significant when pain dominates the presentation. Fifth, the metabolic side‑effects, including weight gain and potential dyslipidemia, warrant longitudinal monitoring, especially in populations at risk for metabolic syndrome. Sixth, the risk of overdose toxicity remains higher with Amitriptyline due to its narrow therapeutic index, necessitating caution in prescribing to patients with suicidal ideation. Seventh, the evidence base supporting Amitriptyline’s use in migraine prophylaxis remains stronger than that for many newer agents, with a roughly 50% reduction in migraine frequency reported in multiple randomized trials. Eighth, the tolerability landscape suggests that while Sedation is a frequent complaint, it can be leveraged therapeutically for patients with comorbid insomnia, turning a side‑effect into a therapeutic advantage. Ninth, the decision matrix should incorporate patient lifestyle factors; for individuals whose occupations demand alertness, agents with lower sedative properties, such as Venlafaxine or Duloxetine, may be preferable. Tenth, the emerging role of combination therapy, for instance, augmenting low‑dose Amitriptyline with an SSRI, can sometimes achieve synergistic benefits while mitigating dose‑dependent side effects. Eleventh, the importance of shared decision‑making cannot be overstated: patients should be fully informed about the spectrum of potential adverse effects ranging from dry mouth to cardiac arrhythmias. Twelfth, clinicians must remain vigilant for signs of serotonin syndrome when combining Amitriptyline with other serotonergic agents. Thirteenth, real‑world adherence data indicate that despite its side‑effect profile, Amitriptyline maintains higher continuation rates in chronic pain cohorts compared to many newer antidepressants. Fourteenth, the cost factor often makes Amitriptyline an attractive option in resource‑limited settings, being widely available as a generic medication. Finally, the evolving landscape of non‑pharmacologic interventions, such as CBT, should be integrated into treatment plans to provide a holistic approach to depression and chronic pain management.
Krysta Howard
November 24, 2025 AT 19:08Listen, the data is crystal clear – Amitriptyline isn’t some relic you should automatically discard. It stomps the competition in neuropathic pain, and the side‑effects, while real, are manageable with proper monitoring. If you’re scared of the dry mouth, hydrate like a champ; if drowsiness creeps in, adjust dosing time. Don’t let the hype around newer SSRIs blind you from a drug that still delivers solid results. 👊
nica torres
December 4, 2025 AT 19:08Hey everyone, just wanted to say that this guide is super helpful! If you’re dealing with stubborn nerve pain, Amitriptyline can be a real game‑changer. And if you’re worried about feeling sleepy, try taking it at night – it can double as a sleep aid. Keep pushing forward, you’ve got this!
Dean Marrinan
December 14, 2025 AT 19:08Oh sure, because we all love scrolling through another glorified drug list, right? 🙄 But hey, if you enjoy the thrill of balancing cardiac risk against a sprinkle of drowsiness, Amitriptyline is your ticket. Meanwhile, the SSRIs are just sipping tea, pretending to be the safe choice. In reality, the old‑school TCA still kicks butt for pain, and that’s the juicy part nobody likes to admit.
Oluseyi Anani
December 24, 2025 AT 19:08Friends, let's be clear: the science behind Amitriptyline's efficacy is solid, and dismissing it in favor of trendy newer agents without reviewing the data is, frankly, irresponsible. The table you provided accurately reflects its superior performance in neuropathic pain, and any clinician who overlooks this is missing the forest for the trees. Keep the conversation evidence‑based.
Rahul yadav
January 3, 2026 AT 19:08Reading this blew my mind 😢 – the way Amitriptyline can soothe that relentless nerve ache feels like a warm hug after a cold night. I’ve felt the weight lift when the dosage finally settled. It’s a bittersweet journey, but knowing there’s a medication that truly listens to my pain makes the struggle worthwhile 🌟.
Ryan Pitt
January 13, 2026 AT 19:08Nice breakdown. If you need a quick answer: Amitriptyline = strong pain relief, more side effects. Newer SSRIs/SNRIs = milder side effects, similar mood lift. Choose based on what matters most to you.
Jami Johnson
January 23, 2026 AT 19:08Building on the earlier point about emotional impact, it’s striking how a medication that can cause drowsiness also offers a sense of calm that resonates deeply with those battling chronic pain. The dramatic shift from sleepless nights to a more rested state can transform not just the physical symptoms but also the psychological outlook. When patients share that they finally feel a flicker of hope, it underscores the therapeutic value that goes beyond mere numbers on a table.
Kasey Krug
February 2, 2026 AT 19:08The prior comment romanticizes a drug that carries real cardiac risks. While anecdotal relief is noted, the pharmacological profile of Amitriptyline demands rigorous monitoring, particularly in populations with pre‑existing heart conditions. Overlooking these hazards in favor of emotional narratives can lead to preventable adverse events. A balanced appraisal must weigh both subjective improvement and objective safety data.
jake cole
February 12, 2026 AT 19:08Enough with the sugar‑coated praise – Amitriptyline is a hazardous relic that should be banished from first‑line therapy. Its anticholinergic burden, overdose potential, and cardiac toxicity make it an unacceptable risk when safer alternatives exist. Stop glorifying danger and upgrade your prescriptions.
Natalie Goldswain
February 22, 2026 AT 19:08i love the guide it s super helpful