Retinal Vein Occlusion: Risk Factors and Injection Treatments Explained

Imagine waking up one morning and noticing your vision is blurry-just in one eye. No pain, no redness, no headache. Just a sudden, unexplained fog over part of your sight. That’s how many people discover they have retinal vein occlusion (RVO). It’s not rare. Around 16 million people worldwide live with it. And while it sounds scary, treatment has come a long way-especially when it comes to injections.
What Exactly Is Retinal Vein Occlusion?
Your retina is like the film in a camera. It catches light and turns it into signals your brain reads as images. Blood flows through tiny veins in the retina to keep it alive. When one of those veins gets blocked, fluid leaks into the retina, swelling the macula-the part responsible for sharp central vision. That’s retinal vein occlusion. There are two main types:- Central Retinal Vein Occlusion (CRVO): The main vein behind the eye gets blocked. Vision loss is usually more severe.
- Branch Retinal Vein Occlusion (BRVO): A smaller branch gets blocked. You might lose vision in just one part of your eye, like the top or bottom.
Who’s Most at Risk?
Age is the biggest factor. Over 90% of CRVO cases happen in people over 55. More than half of all RVO cases are in those over 65. But it’s not just an older person’s disease. About 5-10% of cases occur in people under 45. Here’s what raises your risk:- High blood pressure: Present in up to 73% of CRVO patients over 50. Uncontrolled hypertension is the #1 driver.
- High cholesterol: About 35% of RVO patients have total cholesterol above 6.5 mmol/L.
- Diabetes: Affects about 10% of patients over 50 and makes recovery harder.
- Glaucoma: High pressure inside the eye increases risk, especially if the blockage is near the optic nerve.
- Smoking: Found in 25-30% of cases. It damages blood vessels and thickens the blood.
- Obesity and inactivity: Both contribute to poor circulation and artery hardening.
- Blood disorders: In younger patients, conditions like polycythemia vera, leukemia, or inherited clotting disorders (like factor V Leiden) can trigger RVO.
- Birth control pills: For women under 45, oral contraceptives are the most common link to CRVO.
How Are Injections Used to Treat RVO?
There’s no way to unblock the vein. But we can treat the damage it causes: macular edema-the swelling that blurs your vision. The go-to treatment? Injections into the eye. Yes, that sounds intense. But it’s quick, safe, and often life-changing. Two main types of injections are used:Anti-VEGF Injections
These block a protein called VEGF that causes leaking blood vessels and swelling. Three drugs are commonly used:- Ranibizumab (Lucentis): Approved for RVO in 2010.
- Aflibercept (Eylea): Approved in 2012. Often more effective in severe cases.
- Bevacizumab (Avastin): Originally a cancer drug, now used off-label. Costs about $50 per shot vs. $2,000 for the others.
- In the BRAVO trial, patients on ranibizumab gained an average of 16.6 letters on an eye chart after a year. The placebo group gained just 7.4.
- Aflibercept in the COPERNICUS trial improved vision by 18.3 letters on average.
Corticosteroid Injections
The dexamethasone implant (Ozurdex) is a tiny, dissolving pellet injected into the eye. It slowly releases steroid over 3-6 months. It’s not first-line, but it helps when anti-VEGF doesn’t work:- In the GENEVA study, 27.7% of CRVO patients gained 15+ letters of vision with Ozurdex vs. 12.9% with placebo.
- One patient on Reddit said: "After 8 Avastin shots with no change, Ozurdex gave me 10 lines back. Worth every penny."
- 60-70% of patients with natural lenses develop cataracts faster.
- 30% get elevated eye pressure, needing extra meds.
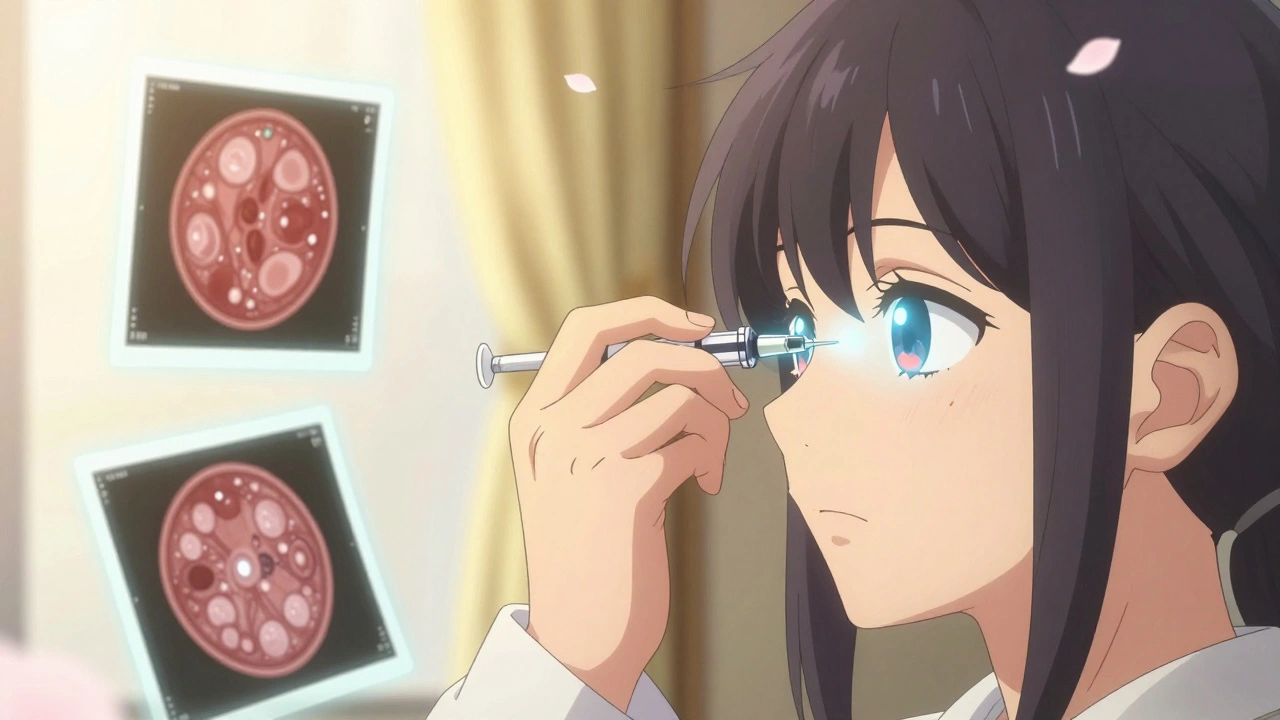
What’s the Procedure Like?
You might be nervous. But here’s what actually happens:- You sit in a chair, head stabilized.
- Your eye is numbed with drops.
- The doctor cleans the surface with antiseptic.
- A tiny speculum holds your eyelid open.
- The needle goes in-quick, sharp pressure, then it’s over.
- It takes less than 10 minutes.
How Do Doctors Know If It’s Working?
They use optical coherence tomography (OCT). This non-invasive scan shows the thickness of your retina. Treatment starts when central subfield thickness (CST) is above 300 micrometers. The goal? Get it below 250. If CST stays high after 3 months, your doctor might switch drugs or add steroids. Vision improvement takes time. Most patients see gains within 1-3 months. About 30-40% reach 20/40 vision or better after a year of treatment.What Are the Real-Life Challenges?
The science works. But life doesn’t always cooperate.- Cost: Lucentis and Eylea cost $2,000 per shot. Even with insurance, copays can hit $150-$500. Avastin is cheaper, but not always covered.
- Frequency: Monthly shots for months. That’s 12+ trips to the clinic a year. Many patients miss appointments because of anxiety, transportation, or work.
- Emotional toll: "The waiting room is full of people who’ve been here before. I know the drill, but my heart still races every time," one patient wrote on Reddit.
- Treatment fatigue: After 18 months of injections, some patients stop going-even when their vision is still improving.

What’s Next in RVO Treatment?
The future is about less frequent treatment and smarter choices.- Treat-and-extend: Start with monthly shots, then stretch the time between them if the eye stays stable. One 2023 study showed this works just as well as monthly, with 30% fewer injections.
- Port Delivery System: A tiny implant (Susvimo) placed in the eye that slowly releases ranibizumab. Approved for AMD, now being tested for RVO. Could mean injections every 6 months instead of monthly.
- Gene therapy: RGX-314 is in trials. It’s a one-time injection that makes your eye produce its own anti-VEGF protein.
- Combination therapy: Some doctors now use anti-VEGF + steroid together for stubborn cases.

Jordan Wall
December 3, 2025 AT 23:33So essentially, RVO is just a vascular thrombotic event in the retinal microcirculation, right? 🤔 The VEGF cascade is the real villain here-anti-VEGF agents like aflibercept are the gold standard, but let’s be real, the cost-benefit analysis is a total dumpster fire in the US healthcare system. 🤯 Avastin? Off-label but clinically equivalent? Of course it is. Pharma’s just milking the patent treadmill. 🏥💸
Ben Choy
December 4, 2025 AT 10:15I had BRVO last year. Honestly? The injections were way less scary than I thought. The numbing drops do the trick, and it’s over before you blink. I cried because I was nervous, not because it hurt. 😅 My vision went from ‘can’t read the clock’ to ‘reading my grandkid’s handwriting’ in 3 months. Stay consistent. It’s worth it.
Emmanuel Peter
December 4, 2025 AT 17:34Let’s cut through the fluff. You’re telling me 73% of CRVO patients have hypertension? Shocking. 😒 And yet, nobody’s talking about how 80% of those patients were told to ‘eat less salt’ and then ignored it for 15 years. This isn’t a medical mystery-it’s a behavioral failure. You want to avoid RVO? Stop being lazy. Check your BP. Lose weight. Quit smoking. Done. No magic injections needed if you’d just taken care of yourself.
Ashley Elliott
December 5, 2025 AT 22:24Thank you for writing this with such clarity. I’m a nurse who’s seen patients terrified of eye injections-and I’ve seen them regain their lives because of them. 🫶 The emotional toll is real: the waiting room anxiety, the fear of the needle, the guilt when you miss an appointment because you can’t afford the Uber. But please, if you’re reading this and you’re scared? Go. One shot at a time. You’re not alone. Your vision matters.
Chad Handy
December 5, 2025 AT 23:45Look, I’ve been through 22 anti-VEGF injections over 21 months. I’ve had Ozurdex. I’ve had OCTs. I’ve had the red eye, the floaters, the panic attacks before every appointment. And I’ll tell you this: the system is designed to break you. The cost? $30,000 a year if you’re on Eylea. The time? Half a day off work every month. The emotional weight? You start dreading your own eyes. I’m 48. I’m not a statistic. I’m a guy who can’t drive at night anymore because I’m scared I’ll miss a stop sign. And yes, the injections helped-but they didn’t fix the system that makes me choose between groceries and my vision. Someone needs to fix this. Not me. Not my doctor. Someone with power.
Ollie Newland
December 6, 2025 AT 03:01Anti-VEGF therapy is the standard, no doubt. But the real game-changer is treat-and-extend. I’ve been on it for a year-started monthly, now I’m at 10-week intervals. OCT shows stable CST under 240. Fewer trips, same results. And honestly? The clinic staff noticed I’m not showing up as often and actually complimented me on my adherence. 😅 It’s not just about the drug-it’s about smart, individualized management. Also, Avastin is still the unsung hero. $50 vs $2K? If your insurance covers it, push for it.
Rebecca Braatz
December 6, 2025 AT 20:15STOP WAITING. If you’ve got blurry vision in one eye? Go to the ER or an ophthalmologist TODAY. Not tomorrow. Not next week. TODAY. This isn’t a ‘maybe it’ll clear up’ situation. Every day you wait, you’re losing more photoreceptors. I’m not being dramatic-I’ve seen people who waited too long and lost 70% of their vision permanently. You don’t get a second chance with the retina. Get checked. Now. Your future self will thank you.
Benjamin Sedler
December 8, 2025 AT 07:25Okay but what if it’s not hypertension? What if it’s a secret clotting disorder? What if you’re 39, work out daily, eat kale, and still get CRVO because your mom had Factor V Leiden? 🤷♂️ The whole ‘lifestyle causes RVO’ narrative is so reductive. I got this after a 10-hour flight. My BP was perfect. Cholesterol? Normal. No smoking. No diabetes. So yeah, let’s stop blaming the patient and start asking why the screening protocols ignore younger, healthy people. The system is failing them.
Heidi Thomas
December 9, 2025 AT 01:48