Meglitinides and Hypoglycemia: Why Skipping Meals Is Dangerous with These Diabetes Drugs

Meglitinides Hypoglycemia Risk Calculator
How to Use This Tool
Enter when you take your medication and when you plan to eat. This calculator will show your risk of hypoglycemia based on the time between your dose and meal. Remember: Meglitinides only work when taken 15 minutes before eating!
Your Risk Assessment
Important: This tool is for educational purposes only. Always consult your doctor for medical advice.
Safety Recommendations
When you’re managing type 2 diabetes, taking medication at the right time isn’t just about following a schedule-it’s about staying alive. That’s especially true for meglitinides, a class of diabetes drugs designed to help control blood sugar after meals. But here’s the catch: if you skip a meal after taking one, your blood sugar can crash-fast.
What Are Meglitinides and How Do They Work?
This speed is the whole point. They’re meant for people who don’t eat at the same time every day-someone who works night shifts, has unpredictable meals because of travel or illness, or just doesn’t feel hungry at the same time each morning. The idea is simple: take the pill 15 minutes before you eat, and your body releases just enough insulin to handle the food you’re about to consume.
But if you don’t eat? That same insulin has nothing to act on. And that’s when things go wrong.
The Hidden Danger: Hypoglycemia When Meals Are Skipped
Hypoglycemia-low blood sugar-is the biggest risk with meglitinides. And it’s not just a mild inconvenience. A blood sugar drop below 70 mg/dL can cause shaking, sweating, confusion, dizziness, or even seizures and loss of consciousness. In older adults or people with heart disease, it can trigger a heart attack.
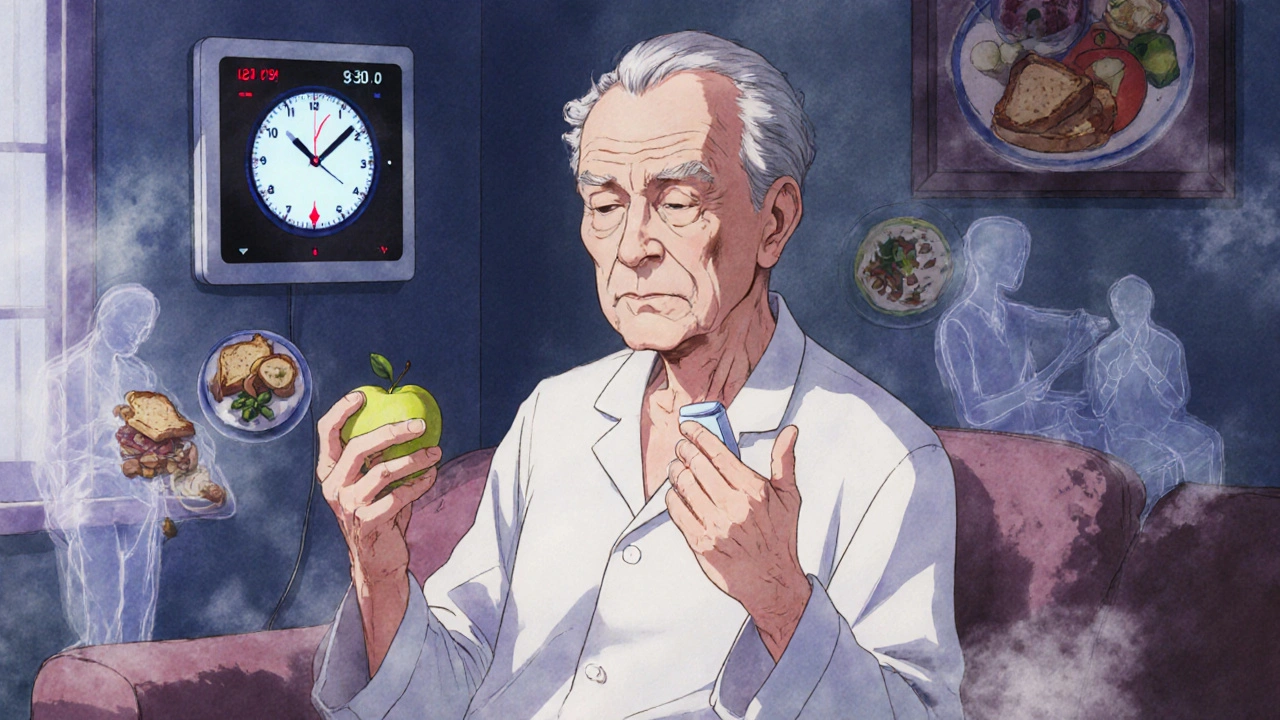
Studies show that skipping just one meal after taking a meglitinide increases your risk of hypoglycemia by nearly 4 times. For someone taking repaglinide at 8 a.m. and not eating until noon, the drug peaks at 9:30 a.m.-and that’s when your blood sugar starts plummeting. You might feel fine until you suddenly can’t think straight. That’s not a guess-it’s what happened in clinical trials. One 2017 study found that 41% of all hypoglycemic events in meglitinide users occurred between 2 and 4 hours after dosing-the exact window when the drug is strongest and food is missing.
This isn’t a rare side effect. About 1 in 5 people taking meglitinides will experience at least one episode of low blood sugar in a year. And if you’re over 65, have kidney problems, or take other diabetes meds like insulin or sulfonylureas, your risk jumps even higher.
Why Are Older Adults and People With Kidney Disease at Higher Risk?
Older adults often have trouble remembering meals. They might skip lunch because they’re not hungry, or eat dinner late because they’re tired. That’s dangerous with meglitinides. The American Diabetes Association’s 2025 guidelines specifically warn that older adults face a higher risk of hypoglycemia “for many reasons, including irregular meal intake.”
Kidney disease makes it worse. Most diabetes drugs are cleared by the kidneys, but meglitinides are mostly broken down by the liver. That’s why repaglinide is often preferred over sulfonylureas for people with kidney issues. But even then, the risk of low blood sugar is still 2.4 times higher in people with advanced kidney disease compared to those without it. The body can’t adjust insulin levels as well when organs are damaged. So even if you eat on time, your system might still overreact.
Meglitinides vs. Other Diabetes Drugs: What’s the Difference?
Let’s compare meglitinides to other common diabetes pills:
| Drug Class | Duration of Action | Hypoglycemia Risk with Missed Meals | Best For |
|---|---|---|---|
| Meglitinides (repaglinide, nateglinide) | 2-4 hours | Very high if meals skipped | Irregular meal schedules |
| Sulfonylureas (glipizide, glyburide) | 12-24 hours | High, even with regular meals | Consistent daily routines |
| Metformin | 24+ hours | Very low | First-line treatment, most patients |
| GLP-1 agonists (semaglutide, liraglutide) | 1-7 days | Low unless combined with insulin | Weight loss + blood sugar control |
Metformin doesn’t cause hypoglycemia at all. That’s why it’s the first drug most doctors prescribe. Sulfonylureas are risky because they keep working all day-even if you skip breakfast. But meglitinides are different: they’re only dangerous if you forget to eat right after taking them. That’s why they’re still used-when someone’s schedule is too unpredictable for anything else.
How to Use Meglitinides Safely
If you’re on repaglinide or nateglinide, here’s what you need to do:
- Take it 15 minutes before you eat. Don’t wait. Don’t guess. If you’re not eating in the next 15 minutes, don’t take the pill.
- Never skip a meal after taking it. Even if you’re not hungry, eat something small-a piece of fruit, a handful of nuts, a slice of toast. Empty stomach + meglitinide = dangerous drop.
- Carry fast-acting sugar. Always have glucose tablets, juice, or candy on you. If you feel shaky or dizzy, treat it immediately.
- Use a reminder app. Studies show that phone reminders cut hypoglycemia events by 39%. Set a daily alarm for meals and medication.
- Ask about CGM. Continuous glucose monitors (CGMs) track your blood sugar in real time. For meglitinide users with irregular meals, CGMs reduce low-blood-sugar episodes by 57%.
Some doctors recommend the “dose-to-eat” method: only take the pill when you know you’re about to eat. No meal? No pill. That’s safer than taking it on a fixed schedule and hoping you remember to eat.
What’s Next for Meglitinides?
Meglitinides aren’t going away-but they’re not growing fast either. Only about 4.2% of people with type 2 diabetes in the U.S. use them. Newer drugs like GLP-1 agonists (semaglutide, tirzepatide) are more popular because they help with weight loss and have lower hypoglycemia risk.
But for people who can’t tolerate those drugs or need flexible dosing, meglitinides still matter. Researchers are working on extended-release versions of repaglinide. Early trials show a new slow-release formula cuts hypoglycemia by 28% while keeping meal-time flexibility. That could be a game-changer.
For now, though, the rule is simple: Take it before you eat. Don’t eat? Don’t take it. That’s the only way to stay safe.
Can I take meglitinides if I skip meals often?
Only if you’re willing to adjust your dosing. Meglitinides are designed for irregular schedules, but they require you to match each dose with a meal. If you skip meals frequently and can’t reliably eat within 15 minutes of taking the drug, this medication isn’t safe for you. Talk to your doctor about alternatives like metformin or GLP-1 agonists.
What should I do if I forget to eat after taking meglitinide?
Check your blood sugar immediately. If it’s below 70 mg/dL, consume 15 grams of fast-acting carbs-like 4 ounces of juice, 3-4 glucose tablets, or 1 tablespoon of sugar. Recheck in 15 minutes. If it’s still low, repeat. Call your doctor if you’ve had more than one episode in a week. Never take another dose until you’ve eaten a full meal.
Is repaglinide safer than nateglinide for kidney patients?
Yes. Repaglinide is mostly broken down by the liver, not the kidneys, so it’s preferred for people with advanced kidney disease. However, the dose must be reduced-usually to 60 mg per meal instead of 120 mg. Nateglinide is cleared more by the kidneys, so it’s less ideal if your kidney function is low. Always follow your doctor’s dosing instructions.
Can I take meglitinides with insulin?
It’s possible, but it’s risky. Combining meglitinides with insulin significantly increases hypoglycemia risk. If your doctor prescribes both, you’ll need tighter meal planning, frequent blood sugar checks, and likely a CGM. Never combine them without close medical supervision.
Do meglitinides cause weight gain?
Yes, they can. Like other insulin-stimulating drugs, meglitinides can lead to weight gain because insulin promotes fat storage. If weight is a concern, your doctor might suggest GLP-1 agonists instead-they help you lose weight while controlling blood sugar.
Bottom Line
Meglitinides are a tool-not a fix. They work great when your meals are unpredictable. But they demand precision. Take them before you eat. Eat something. Don’t skip meals. If you can’t do that, they’re not the right drug for you. The risk of low blood sugar isn’t theoretical. It’s real, dangerous, and preventable. Talk to your doctor about your schedule, your habits, and your real-life routine. The best diabetes treatment isn’t the one with the most science-it’s the one you can actually live with safely.

Ganesh Kamble
October 30, 2025 AT 15:04So let me get this straight-you take a pill that makes your pancreas go full insulin mode, then you forget to eat and suddenly you’re a shaking mess? That’s not medicine, that’s a Russian roulette game with your brain. I’ve seen people pass out at their desks because they thought ‘I’ll just skip lunch today.’ Spoiler: your liver doesn’t care about your diet plan.
Jenni Waugh
November 1, 2025 AT 09:30Oh sweet mercy. Another ‘diabetes is a lifestyle choice’ lecture wrapped in clinical jargon. Let me guess-this was written by someone who’s never had to choose between paying rent and buying glucose tablets? You tell me to eat a piece of fruit after taking repaglinide, but what if I’m homeless? Or working two jobs? Or just plain broke? This isn’t advice. It’s privilege in a lab coat.
Theresa Ordonda
November 3, 2025 AT 05:15YESSSS this is why I HATE when doctors push these drugs without context 😤🫠 I had my cousin on nateglinide and she skipped her breakfast because she was ‘not hungry’-and then she called 911 at 10 a.m. because she thought the ceiling was breathing. CGMs are not optional. They’re survival gear. Like a seatbelt for your pancreas. 🚨🩸
Judy Schumacher
November 5, 2025 AT 01:35It is, in fact, a remarkable oversight in contemporary endocrinological practice that clinicians continue to prescribe meglitinides to patients whose socioeconomic status, cognitive capacity, or temporal consistency renders adherence to the ‘dose-to-eat’ protocol fundamentally unfeasible. The pharmacokinetic profile of repaglinide, while elegant in theory, is catastrophically mismatched with the lived reality of millions who must prioritize survival over precision. One is left to wonder: is this innovation-or institutional negligence dressed in white coats?
Megan Raines
November 6, 2025 AT 00:47So… you’re telling me the solution to ‘I forget to eat’ is to… eat? Wild. 🤔 I mean, I get it, but like… why is this even a thing we need a 2000-word essay for? My grandma takes metformin and lives fine. Maybe the real problem isn’t the drug-it’s the expectation that everyone’s life looks like a corporate wellness brochure.
Mamadou Seck
November 6, 2025 AT 03:06bro why are we even talking about this like its rocket science its literally take it before you eat if you dont eat dont take it why do we need studies and tables and graphs its common sense
chantall meyer
November 7, 2025 AT 07:14How quaint. In my village, we just ate when the sun was high and slept when it set. No pills. No apps. No CGMs. Modern medicine thinks it can outsmart biology. It cannot.
Lorne Wellington
November 7, 2025 AT 15:26Hey everyone-big love to the OP for breaking this down so clearly 🙌 I’ve been a diabetes educator for 12 years and this is exactly what I tell my patients: meglitinides = precision tools, not magic bullets. If you’re juggling work, kids, or chronic fatigue, talk to your doc about metformin or GLP-1s. And PLEASE get a CGM if you can-it’s like having a personal bodyguard for your blood sugar 🛡️💙
Will RD
November 8, 2025 AT 19:24you say dont take it if you dont eat but what if you forget and take it anyway then what do you do i mean really
Jacqueline Anwar
November 8, 2025 AT 23:47It is both alarming and deeply concerning that the medical community continues to normalize the use of pharmacological agents that demand such a high degree of behavioral compliance from populations demonstrably incapable of sustaining it. This is not patient-centered care. This is pharmaceutical convenience disguised as therapeutic innovation.
California Daughter
November 9, 2025 AT 21:29Okay, but… what if you’re just… not hungry? Like, genuinely? I’ve been on this drug for 6 months and sometimes I wake up and my stomach just… doesn’t care. Do I force-feed myself a banana just so my pancreas doesn’t revolt? I feel like this is just… gaslighting me into eating? 🤔