Medication Reformulations: When Companies Change Drug Formulas

Dosing Frequency Impact Calculator
How Dosing Frequency Affects Adherence
Research shows that reducing dosing frequency can significantly improve adherence. Based on clinical studies, switching from multiple daily doses to once-daily dosing can reduce missed doses by up to 40%.
How this works: According to clinical studies, reducing dosing frequency from multiple daily doses to once daily can reduce missed doses by up to 40%. This calculator uses that estimate to show potential improvements in your adherence when switching to a reformulated version.
Have you ever noticed your prescription pill looks different - maybe smaller, or in a new shape - and wondered why? Or maybe your doctor switched your injection to a pill, and you were told it’s the same medicine? That’s not a mistake. It’s medication reformulation.
Companies don’t change drug formulas just to make things look new. They do it to make medicines work better, be easier to take, or last longer on the market. And while it sounds simple, the science behind it is complex, tightly regulated, and often makes a real difference in how patients feel and stick to their treatment.
What Exactly Is a Reformulation?
A reformulation isn’t a new drug. It’s the same active ingredient - the part that actually treats your condition - but changed in how it’s made. Think of it like rewriting a recipe. The main ingredient stays the same, but maybe you swap out sugar for honey, change the cooking time, or serve it in a different form.
Common changes include:
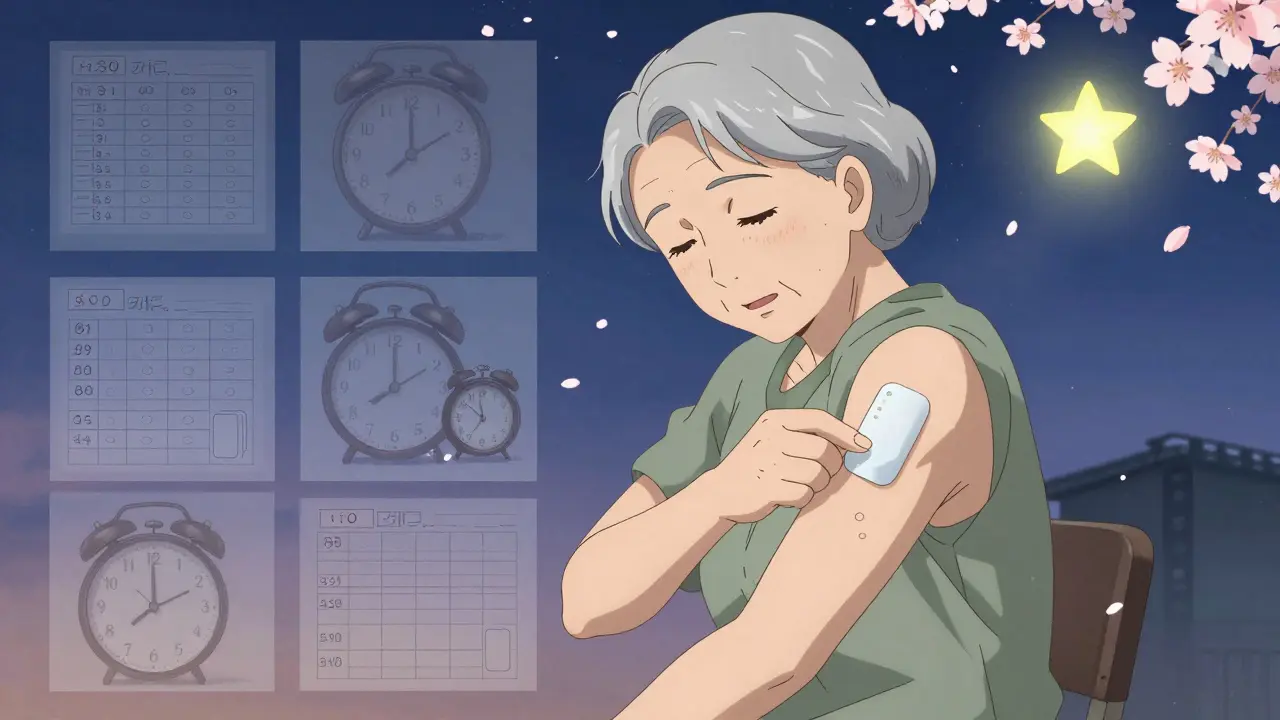
- Switching from a pill you swallow to a patch you stick on your skin
- Making a tablet dissolve slower so you don’t have to take it 4 times a day
- Removing a dye or filler that causes allergic reactions in some people
- Changing the size or shape of a pill to make it easier to swallow
- Turning a liquid medicine into a powder you mix at home
The key rule? The active ingredient must stay chemically identical. If the molecule itself changes, it’s not a reformulation - it’s a new drug. That’s why a chiral switch (switching from one mirror-image version of a molecule to another) counts as a reformulation, but turning a drug into a completely different chemical compound doesn’t.
Why Do Companies Do This?
It’s not just about profit. While extending patent life is part of the business case, the real driver is patient needs.
After a drug hits the market, doctors and patients learn things the clinical trials never showed. Maybe people forget to take it because it’s too frequent. Maybe it causes stomach upset. Maybe it’s hard to store. Reformulation fixes those problems.
Take a diabetes drug originally given as a daily injection. A reformulated version might now be a once-weekly pill. That’s not just convenient - it’s life-changing for someone who struggles with needles. Or consider a painkiller that used to cause nausea. A reformulated version with a new coating can cut that side effect by 60%.
For rare diseases, reformulation is often the only way to make treatment work. An orphan drug might have been designed for adults, but kids can’t swallow the pill. A reformulation into a liquid or dissolvable tablet makes it usable. That’s not a marketing gimmick - it’s medical necessity.
How Is It Approved?
The FDA has a special path for this: the 505(b)(2) pathway. It lets companies skip repeating every single study done on the original drug. They can use existing safety and effectiveness data - as long as they prove their new version works the same way.
That means reformulations don’t need 10 years and $2.6 billion to get approved. Most take 3-5 years and cost between $50 million and $100 million. Compare that to a brand-new drug, and you see why so many companies choose this route.
But there’s a catch. If the reformulation changes how the drug is absorbed - say, from fast-acting to slow-release - the company still needs to run clinical trials to prove it’s safe and effective. The FDA doesn’t cut corners on safety.
One thing they do check closely: bioequivalence. That means your body absorbs the reformulated version at the same rate and to the same extent as the original. If it doesn’t, the drug won’t work the same - and could even be dangerous.

Real-World Impact: What Changes Actually Matter
Not all reformulations are equal. Some make a huge difference. Others? Barely noticeable.
Here’s what actually improves lives:
- Reducing dosing frequency - Going from 3 pills a day to 1 cuts missed doses by up to 40%, according to studies.
- Changing delivery method - Switching from injection to oral form improves adherence by 50% or more in chronic conditions.
- Removing allergens - Removing lactose or artificial dyes helps patients with sensitivities avoid rashes, bloating, or worse.
- Improving stability - A reformulation that doesn’t need refrigeration makes it easier to use in hot climates or rural areas.
On the flip side, some reformulations are barely more than a new color or capsule shape. These are called “evergreening” tactics - small tweaks designed to block generics without improving care. The FDA has cracked down on these, especially when they don’t change absorption or patient outcomes.
The real winners? Reformulations that solve real problems. Like a seizure medication that used to require precise timing. A reformulated extended-release version lets patients take it once at bedtime - no more midnight alarms.
Who Benefits the Most?
It’s not just big pharma. Reformulation helps:
- Pediatric patients - Kids can’t swallow big pills. Reformulations into flavored liquids or chewables make treatment possible.
- Seniors - Swallowing difficulties, memory lapses, and polypharmacy make simple dosing critical.
- People in low-resource areas - A reformulation that doesn’t need cold storage can reach remote clinics.
- Patients with rare diseases - Often, there’s only one approved drug. Reformulation is the only way to make it work better.
For example, a 2022 case study from a mid-sized pharma company showed how reformulating an orphan drug for a rare muscle disorder cut the number of daily doses from 6 to 1. Patient compliance jumped from 58% to 89%. That’s not a statistic - it’s fewer hospital visits, better quality of life, and more time with family.
The Dark Side: When Reformulation Goes Wrong
Most reformulations are safe. But not all.
Sometimes, changing excipients - the inactive ingredients - causes unexpected side effects. A patient who’s been on a drug for years might suddenly get headaches, rashes, or dizziness after switching to a reformulated version. Why? Maybe the new coating interacts with a food they eat. Or a preservative triggers an allergy they never knew they had.
These cases are rare, but they happen. And when they do, it’s often because the bioequivalence tests didn’t catch subtle differences in how the body reacts. The FDA requires bioequivalence, but not always full pharmacodynamic studies - especially if the change seems minor.
That’s why it’s important to report any new symptoms after a pill change. Talk to your pharmacist. Tell your doctor. It might be nothing - or it might be a sign the reformulation isn’t right for you.
What’s Next?
The future of reformulation is getting smarter.
New technologies are letting companies design pills that release medicine only in the right part of the gut. Or patches that deliver steady doses for weeks. Or inhalers that target lungs directly instead of flooding the whole body.
And the FDA is helping. In 2022, they released new guidance to make it easier to approve reformulations for complex drugs - especially those used for rare diseases or in children.
One trend to watch: reformulation of generic drugs. Once a patent expires, companies often reformulate the generic version to make it more stable, easier to take, or cheaper to produce. That’s not cheating - it’s improving access.
By 2026, reformulations will account for nearly one-third of all new drug applications to the FDA. That’s not because companies are lazy. It’s because they’ve learned: sometimes, the best new drug is an old one - done better.
Are reformulated drugs the same as generics?
No. Generics are exact copies of brand-name drugs, made after the patent expires. Reformulations are modified versions of existing drugs - sometimes brand-name, sometimes generic - with changes to how they’re made, delivered, or absorbed. A generic version of a reformulated drug would still have to match the reformulated version’s performance, not the original.
Can a reformulation make a drug less effective?
It’s rare, but possible. If the reformulation changes how the drug is absorbed - for example, by making it dissolve too slowly or too quickly - it might not reach the right level in your blood. That’s why the FDA requires bioequivalence testing. Still, if you notice your symptoms returning or getting worse after a pill change, talk to your doctor. It could be the reformulation.
Why does my pill look different now?
Your pharmacy might have switched to a different manufacturer, or your doctor switched you to a reformulated version. Pill appearance changes often mean the formula was tweaked to improve dosing, reduce side effects, or cut costs. Check the label for the manufacturer name. If you’re unsure, ask your pharmacist - they can tell you if it’s the same drug, just reformulated.
Do reformulated drugs cost more?
Sometimes. If it’s a brand-name reformulation with a new patent, yes - it can be more expensive. But if it’s a reformulated generic, it’s often cheaper. The goal of reformulation isn’t always to raise prices. Often, it’s to improve compliance, which lowers long-term healthcare costs by preventing hospitalizations and complications.
Should I be worried if my medication was reformulated?
Not necessarily. Most reformulations are improvements. But always monitor how you feel. If you notice new side effects, changes in how well the drug works, or unusual reactions, contact your doctor. Don’t assume it’s just in your head. Your body might be telling you the new version doesn’t suit you.
