Medication-Induced Delirium in Older Adults: How to Spot the Signs and Prevent It
What Is Medication-Induced Delirium?
Medication-induced delirium is a sudden, dangerous change in thinking and awareness that happens when certain drugs mess with the brain of an older adult. It’s not dementia. It’s not just being tired. It’s a medical emergency that can come on in hours or days - often after a new pill is started or a dose is changed. Unlike dementia, which gets worse slowly over years, delirium flips on and off like a light switch. One minute, your loved one is clear-headed; the next, they’re confused, agitated, or staring blankly at the wall.
This isn’t rare. About 1 in 5 older adults in the hospital develop delirium, and nearly half of those cases are caused by medications. The worst part? Many doctors and nurses miss it. Because the symptoms look like aging or depression, they’re often ignored - until it’s too late. Patients with delirium stay in the hospital nearly a week longer, are twice as likely to die within a year, and rarely recover their full mental sharpness.
How Do Medications Cause Delirium?
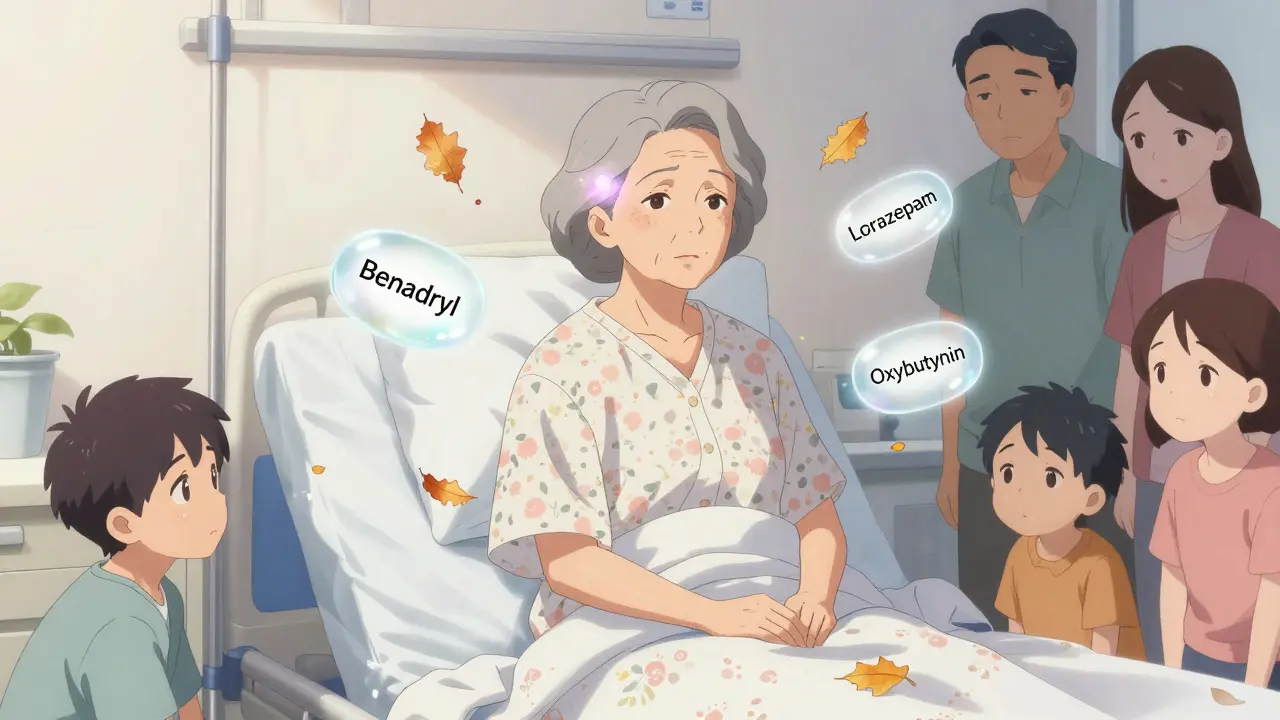
It all comes down to brain chemistry. Older brains are more sensitive to drugs that block acetylcholine - a key neurotransmitter for memory, attention, and alertness. Medications with strong anticholinergic effects - like diphenhydramine (Benadryl), oxybutynin (for overactive bladder), and amitriptyline (for pain or depression) - are the top offenders. Every extra anticholinergic drug you add multiplies the risk. Someone taking three or more of these meds has almost five times the chance of falling into delirium compared to someone taking none.
Benzodiazepines like lorazepam (Ativan) and diazepam (Valium) are just as dangerous. They slow down brain activity so much that the brain can’t process information properly. Even short-term use in the hospital can trigger delirium. And here’s the twist: using them to calm someone down often makes things worse. Instead of soothing, they deepen confusion.
Opioids, especially morphine and meperidine, also play a role. Meperidine is particularly risky because its breakdown product, normeperidine, overstimulates the nervous system. Hydromorphone is a safer alternative - it causes 27% less delirium at the same pain-relieving dose.
What Does It Look Like? The Three Faces of Delirium
Delirium doesn’t always mean shouting and thrashing. In fact, the most common form in older adults is the quiet kind - hypoactive delirium. About 7 out of 10 cases look like this:
- Slowed down, withdrawn, unresponsive
- Sitting silently, not making eye contact
- Appearing depressed or “just tired”
- Not eating, not talking, not recognizing family
This version gets mistaken for depression, dementia, or just “getting old.” But it’s not normal aging. It’s sudden. It’s different from who they were yesterday. Caregivers often say, “They’re not themselves.” And they’re right.
Hyperactive delirium is the scary one - pacing, yelling, pulling at IV lines, hallucinating. Mixed delirium swings between the two. But here’s the hard truth: the quiet type is deadlier because it’s missed. And missed delirium means delayed treatment - and higher death risk.
Which Medications Are Most Likely to Cause It?
The American Geriatrics Society’s Beers Criteria® lists 56 drugs to avoid in older adults because they’re too risky. Here are the top troublemakers:
- First-generation antihistamines: Diphenhydramine (Benadryl), hydroxyzine, chlorpheniramine - even in OTC allergy or sleep aids
- Bladder meds: Oxybutynin, tolterodine, solifenacin - often prescribed for incontinence
- Antidepressants: Amitriptyline, imipramine, paroxetine - especially the older tricyclics
- Benzodiazepines: Lorazepam, diazepam, alprazolam - even for short-term anxiety or sleep
- Antipsychotics: Quetiapine (Seroquel), risperidone - often used off-label for agitation, despite high risk
- Antibiotics: Ciprofloxacin - yes, even some antibiotics can trigger delirium
Second-generation antihistamines like loratadine (Claritin) or cetirizine (Zyrtec) are much safer. They don’t cross the blood-brain barrier as easily. Same with SSRIs like sertraline or escitalopram - they’re better choices than tricyclics for depression.
How to Prevent It - Before It Starts
Prevention isn’t complicated. It’s just rarely done.
- Review every medication. Ask: “Why is this still on the list?” Every pill should have a reason. If it’s been sitting for months, it’s probably not needed.
- Use the Anticholinergic Cognitive Burden (ACB) scale. This tool scores how much each drug contributes to brain fog. A score of 3 or higher means high risk. Ask your pharmacist to run this check.
- Replace high-risk drugs. Swap Benadryl for Claritin. Swap oxybutynin for pelvic floor therapy. Swap lorazepam for non-drug sleep strategies.
- Use the STOPP/START criteria. This is a checklist doctors use to find bad prescriptions and missing ones. It cuts delirium risk by 26%.
- Manage pain without opioids. Use acetaminophen, ice packs, physical therapy, or nerve blocks. Multimodal pain control reduces opioid use by nearly 40% - and cuts delirium risk along with it.
- Don’t stop benzodiazepines cold turkey. If someone’s been on them for weeks, taper slowly over 7-14 days. Sudden withdrawal can cause delirium tremens - a life-threatening form of delirium.
What Hospitals Are Doing - And What You Should Demand
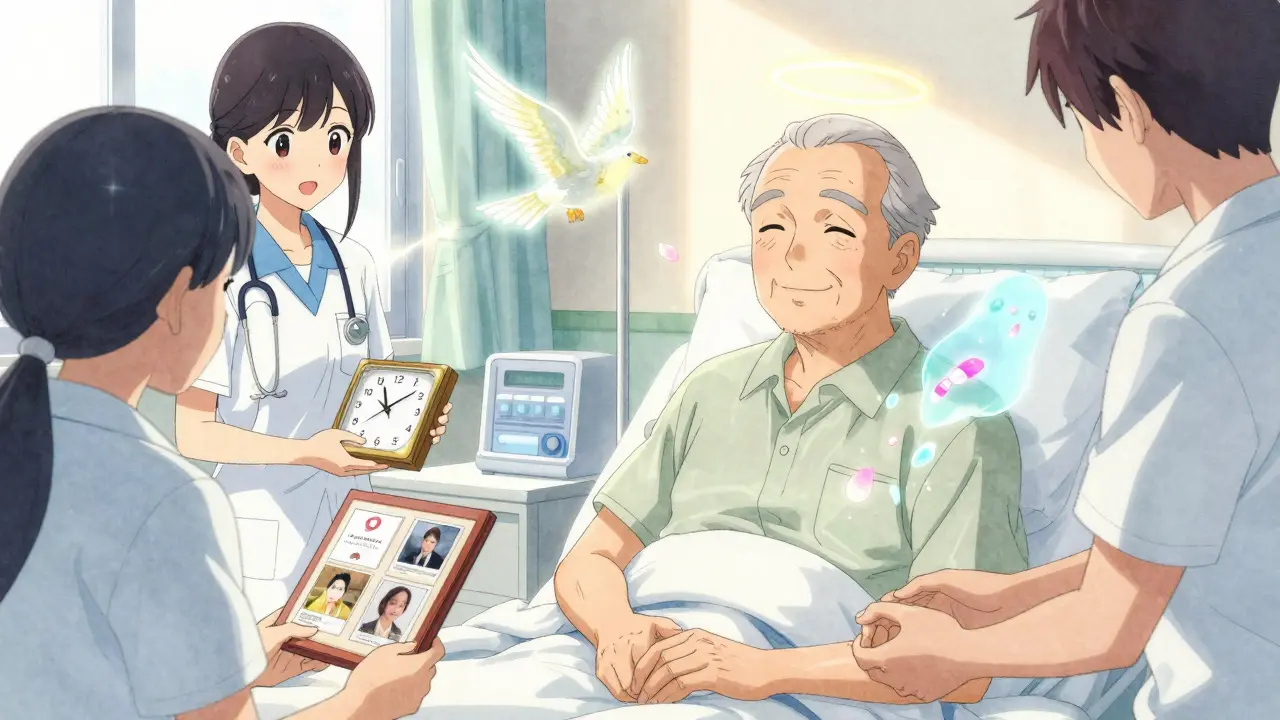
Some hospitals are finally waking up. The Hospital Elder Life Program (HELP), developed at Yale, reduces delirium by 40%. It doesn’t cost much: volunteers help patients stay oriented, get out of bed, drink water, and sleep at night. No drugs needed.
But only 68% of U.S. hospitals have formal delirium prevention plans. And only 18% routinely screen for anticholinergic burden. That’s unacceptable.
Here’s what you can do:
- Ask: “Has my loved one been screened for delirium?”
- Ask: “Can we review all their meds with a pharmacist?”
- Ask: “Are we using the Confusion Assessment Method (CAM) to check for delirium daily?”
- Bring a list of every pill, supplement, and OTC drug they take - including eye drops and patches.
- If they’re in the ICU, ask: “Is this sedative necessary? Can we try less?”
Why This Matters More Than Ever
By 2040, there will be 80 million Americans over 65. That’s 2.3 times more than in 2020. And with more older adults comes more medication use - and more delirium. Right now, medication-induced delirium affects 2.6 million older adults in U.S. hospitals every year. It costs $164 billion annually in extra care, longer stays, and lost independence.
The Centers for Medicare & Medicaid Services now call hospital-acquired delirium a “never event.” That means if you get it in the hospital, they can’t bill you for the extra days. But that doesn’t fix the brain damage.
And here’s the kicker: if your loved one had dementia before, delirium makes it worse - and longer. Their confusion may not go back to baseline. The average delirium episode lasts 8.2 days for someone with dementia - nearly twice as long as for someone without it.
What to Do If You Suspect Delirium
If you notice sudden changes - confusion, withdrawal, agitation, trouble focusing - act fast.
- Don’t wait. Call the nurse or doctor immediately.
- Ask: “Could this be caused by a medication?”
- Bring a full list of all drugs, including supplements and patches.
- Request a medication review and an anticholinergic burden score.
- Push for non-drug interventions: light, movement, familiar faces, clocks, glasses, hearing aids.
Delirium is reversible - if caught early. But every hour you wait makes recovery harder.
Final Thought: You’re the Best Advocate
No one knows your loved one like you do. If they’ve changed - suddenly, sharply - trust that gut feeling. Medications are often the hidden cause. And unlike infections or strokes, this one is preventable. With the right questions, the right reviews, and the right replacements, you can protect their mind - and their future.

Kiran Plaha
January 7, 2026 AT 11:17My grandma started taking Benadryl for sleep and went from sharp as a tack to barely recognizing us in three days. We thought it was dementia. Turned out it was the meds. Took weeks to recover. Never again.
Matt Beck
January 8, 2026 AT 23:07So… we’re just… letting pharmacology run amok in our aging population? 🤔 The brain isn’t a vending machine-you don’t just drop in pills and expect the right snack to come out. It’s a symphony. And we’re playing heavy metal with a kazoo. 🎻💥
Kelly Beck
January 10, 2026 AT 21:47I’m so glad this was posted. My mom was misdiagnosed for months with ‘just depression’ until my sister noticed she hadn’t recognized her own wedding photo in 3 days. We pushed for a med review, found 4 anticholinergics on her list-including a sleep patch she didn’t even know she was using-and within 10 days, she was back to telling jokes and remembering our birthdays. It’s not magic-it’s just common sense. Please, if you’re caring for someone older, sit down with a pharmacist. Not a doctor. A pharmacist. They’re the unsung heroes here.
Molly McLane
January 12, 2026 AT 09:07This is exactly why I started volunteering at the local senior center. I help people organize their meds, print out the Beers Criteria list, and walk them through the ACB scale. One woman had been on oxybutynin for 12 years because her doctor ‘never got around to changing it.’ She hadn’t been herself since 2018. We swapped it for pelvic floor PT. Now she’s gardening again. Small changes. Big impact.
Katie Schoen
January 13, 2026 AT 17:28So let me get this straight: we give old people 7 drugs that turn their brain into a dial-up modem… then act shocked when they ‘go weird’? 😒 I mean, if your phone started lagging after you installed 5 apps you didn’t need, you’d uninstall them. Why is the human brain any different?
Beth Templeton
January 15, 2026 AT 10:09Stop prescribing anticholinergics. Done.
Ryan Barr
January 15, 2026 AT 21:32Delirium is a symptom, not a diagnosis. The real issue is the lack of geriatric training in medical schools. Most physicians are trained to treat diseases, not aging.
Saylor Frye
January 17, 2026 AT 16:50Interesting. But let’s be honest-most of these ‘preventative’ measures are just glorified lifestyle advice wrapped in clinical jargon. You think a 78-year-old with three chronic conditions and no family support is going to ‘swap lorazepam for non-drug sleep strategies’? That’s not prevention. That’s privilege.
Venkataramanan Viswanathan
January 17, 2026 AT 18:13In India, many elderly are given over-the-counter antihistamines for colds or sleep without any medical supervision. Families assume it’s harmless. This article is a wake-up call. We need community pharmacists to step in-not just doctors. Education must reach rural homes, not just urban clinics. The cost of ignoring this is not just medical-it’s cultural. We lose our elders’ wisdom when their minds fade because of a pill they didn’t ask for.
Tiffany Adjei - Opong
January 18, 2026 AT 22:05Wait-so you’re saying the whole medical system is broken because of a few bad drugs? What about dementia? What about stroke? What about the fact that 80% of elderly patients have polypharmacy because they’re sick? This feels like blaming the medicine instead of the aging process. Also, ‘non-drug interventions’ sound nice until you’re trying to calm someone who’s hallucinating at 3 a.m. with no nurse on duty. Just saying.