IBS vs. IBD: What’s the Real Difference Between Functional and Inflammatory Bowel Disorders?

It’s easy to mix up IBS and IBD. Both cause belly pain, bloating, diarrhea, and urgent bowel movements. You might even hear people say, "I have IBS," when they’re really talking about Crohn’s or ulcerative colitis. But here’s the truth: IBS and IBD are not the same thing. One is a malfunctioning system. The other is a damaged one. And the difference changes everything - from how you’re treated to what your future might look like.
IBS: Your Gut Is Working, But It’s Confused
IBS stands for Irritable Bowel Syndrome. It’s not an infection. It’s not cancer. There’s no swelling, no ulcers, no torn tissue. Your colon looks perfectly normal on a colonoscopy. Blood tests come back clean. Scans show nothing wrong. So why do you feel awful?
The problem isn’t structure - it’s signal. Your gut nerves are too sensitive. Your muscles contract too hard or too weak. Food moves too fast or too slow. You feel pain when your intestines stretch normally. That’s IBS.
According to the Rome IV criteria (the gold standard for diagnosis), you have IBS if you’ve had abdominal pain at least one day a week for three months, along with changes in bowel habits. That’s it. No inflammation markers. No tissue damage. Just a misfiring system.
Most people with IBS report bloating (76% of cases), mucus in stool (45%), and symptoms that get worse after eating. Diarrhea-predominant IBS affects 35% of patients. Constipation-predominant? That’s 27%. The rest have a mix of both. Women make up about 65% of IBS cases - no one knows exactly why, but hormones and brain-gut connections likely play a role.
What you won’t find in IBS: blood in your stool, unexplained weight loss, fever, or joint pain. If you have any of those, it’s not IBS. It’s something else - probably IBD.
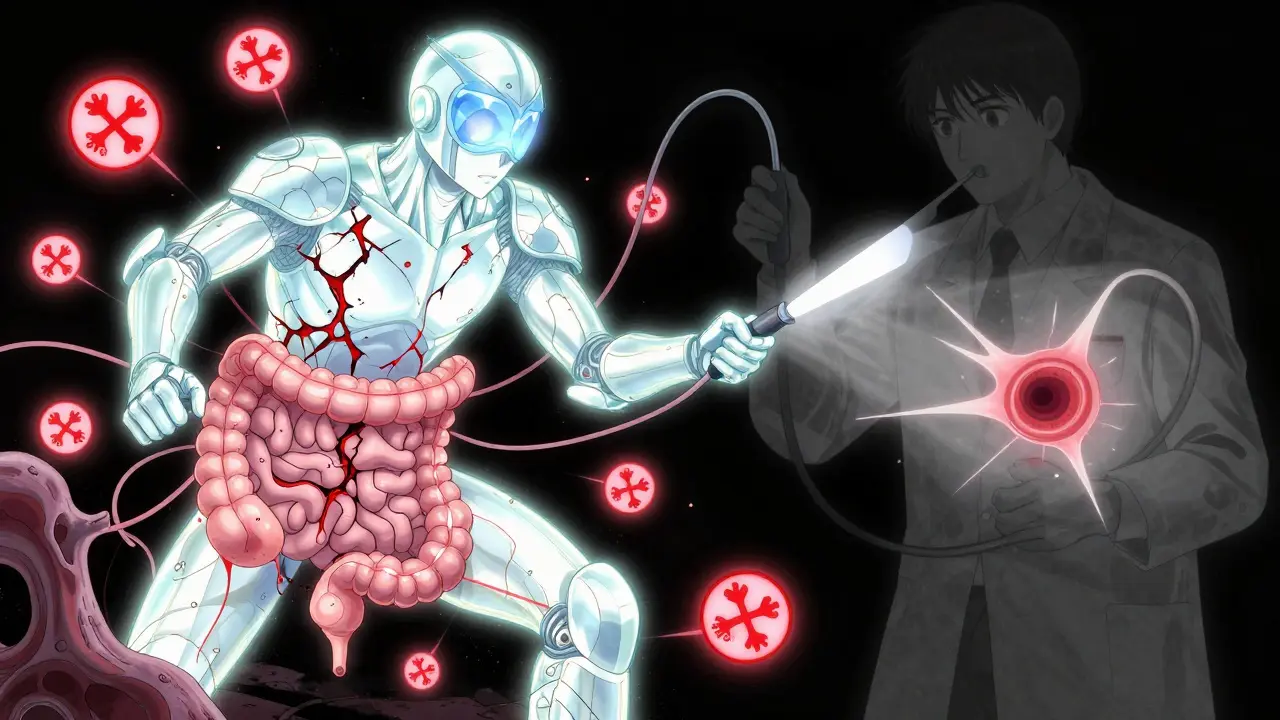
IBD: Your Gut Is Under Attack
IBD - Inflammatory Bowel Disease - is two diseases in one: Crohn’s disease and ulcerative colitis. Both are autoimmune conditions. Your immune system turns on your own gut lining. It doesn’t just irritate it - it destroys it.
In ulcerative colitis, inflammation stays in the colon and rectum. It causes open sores, bleeding, and constant urgency. In Crohn’s, inflammation can hit anywhere from mouth to anus. It burrows deep into the bowel wall, causing thickening, scarring, and tunnels called fistulas.
Here’s what doctors see under the scope: inflamed, red, swollen tissue. Ulcers. Bleeding. Strictures (narrowed sections). In 95% of active IBD cases, fecal calprotectin - a protein released by inflamed white blood cells - is above 250 µg/g. Normal is under 50. CRP levels? Over 5 mg/L in 78% of active cases. Normal is under 3.
IBD symptoms go beyond belly pain. You might lose weight without trying. Have fevers. Notice blood in your stool - bright red or black and tarry. Your joints ache. Your eyes get red and painful. Skin rashes appear. These aren’t random side effects. They’re signs your immune system is firing on all cylinders, even outside your gut.
Left untreated, IBD can lead to serious complications. After 10 years of pancolitis (ulcerative colitis affecting the whole colon), your risk of colorectal cancer jumps by 2% each year. Fistulas and abscesses can require surgery. Toxic megacolon - a life-threatening swelling of the colon - happens in 2-4% of severe ulcerative colitis cases.
The Diagnostic Divide: What Tests Reveal
IBS is diagnosed by ruling everything else out. That’s called a diagnosis of exclusion. Your doctor will check for celiac disease, infections, thyroid problems, and yes - IBD. They’ll order blood tests, stool samples, and likely a colonoscopy. If all those come back normal, and your symptoms match Rome IV criteria, you’ve got IBS.
IBD? That’s confirmed with hard evidence. A colonoscopy with biopsy shows inflammation and damage. MRI enterography finds fistulas or thickened bowel walls. Blood tests reveal elevated CRP and ESR. Fecal calprotectin? High. Very high.
Here’s what’s critical: if you have rectal bleeding, unexplained weight loss, or fever, you don’t wait. You get tested for IBD immediately. The CDC and Mayo Clinic both say: these are red flags. They’re not IBS symptoms. They’re IBD symptoms.
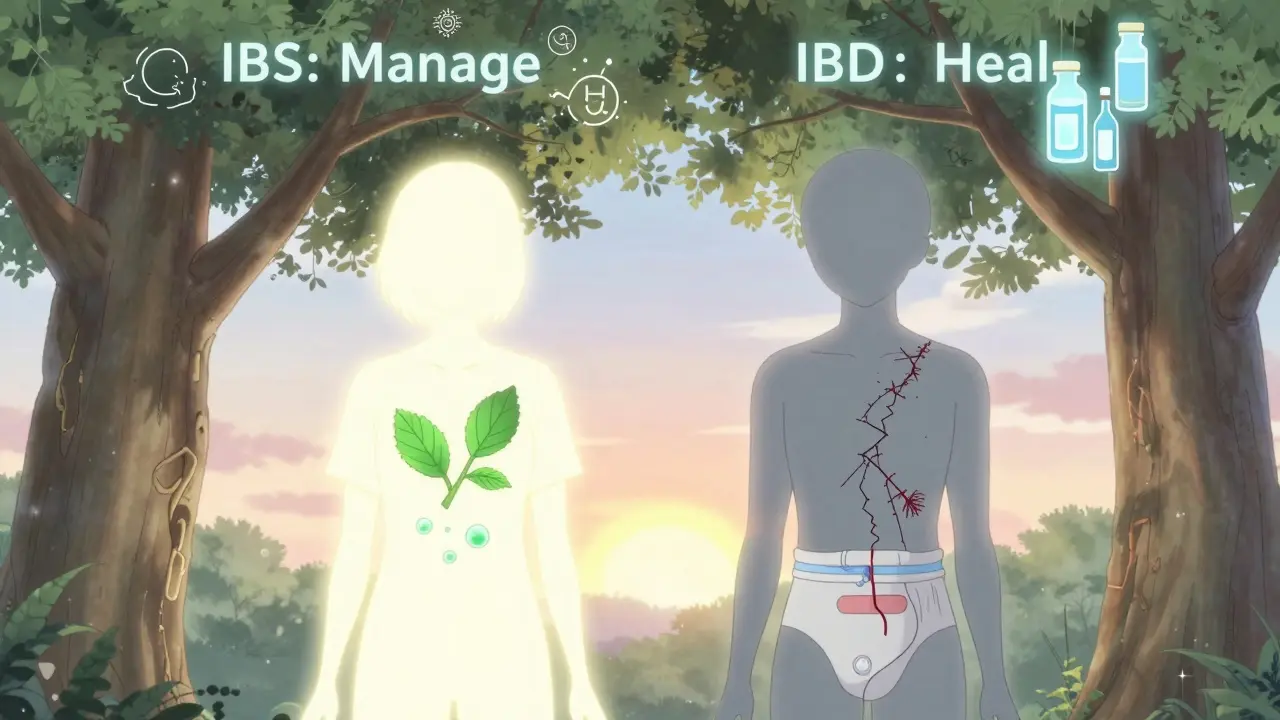
Treatment: Fixing a System vs. Healing Tissue
Because IBS has no physical damage, treatment focuses on calming the system. No pills to cure it - just tools to manage it.
- A low-FODMAP diet helps 76% of people reduce bloating and pain.
- Low-dose antidepressants like amitriptyline reduce pain signals by 50% in 60% of IBS patients.
- Eluxadoline helps with diarrhea-predominant IBS - 35-40% get relief.
- Probiotics, peppermint oil, and stress management (like CBT) also help many.
IBD treatment is completely different. You need drugs that stop your immune system from attacking your gut.
- Anti-TNF drugs like infliximab put 50-60% of Crohn’s patients into remission within 14 weeks.
- Corticosteroids (like prednisone) calm flares fast - but can’t be used long-term due to bone loss, diabetes, and mood swings.
- Vedolizumab targets only the gut, reducing side effects. It puts 48% of ulcerative colitis patients into remission after a year.
- Surgery may be needed: removing the colon for severe ulcerative colitis, or cutting out damaged sections in Crohn’s.
And here’s something many don’t know: you can have both IBS and IBD. Studies show 22-35% of IBD patients in remission still meet IBS criteria. Their gut is healed enough to stop bleeding, but still hypersensitive. That’s why symptom tracking matters - even when you’re "in remission."
What You Can’t Ignore: Long-Term Risks
IBS doesn’t turn into cancer. It doesn’t cause bowel obstructions. It doesn’t lead to surgery. It doesn’t shorten your life. But it can steal your quality of life. People with IBS say they’d give up caffeine, their phone, or even sex to be free of symptoms. That’s how debilitating it can be.
IBD? It can. It does. People with IBD face higher risks of colorectal cancer, liver disease, and bone fractures. They’re more likely to be hospitalized. They need lifelong monitoring. Some need ostomies. Their lives are shaped by the disease - not just managed around it.
But here’s the good news: with modern biologics, many IBD patients now live full, active lives. Remission isn’t just possible - it’s common. The key is catching it early and sticking to treatment.
When to See a Doctor
See a doctor if you have:
- Rectal bleeding - always.
- Unexplained weight loss.
- Fevers that come and go.
- Joint pain or skin rashes along with gut issues.
- Symptoms that started after age 50.
- A family history of IBD or colon cancer.
If you only have bloating, cramps, and changes in bowel habits - and nothing else - IBS is likely. But don’t assume. Get checked. Especially if symptoms are new, worsening, or affecting your sleep, work, or relationships.
Don’t wait for symptoms to get "bad enough." IBD doesn’t always start with a bang. Sometimes it creeps in slowly. By the time you notice blood or weight loss, damage may already be done.
Bottom Line
IBS is a brain-gut communication problem. IBD is an immune system attack. One is managed. The other is treated. One doesn’t damage tissue. The other can destroy it.
Same symptoms? Yes. Same disease? No.
If you’ve been told you have IBS but still have bleeding, fever, or weight loss - get a second opinion. You might have IBD. And if you have IBD and still have bloating and pain after treatment - you might also have IBS. Both can coexist. And both deserve attention.
Your gut isn’t just a pipe. It’s a complex system. And when it’s not working right, you need to know exactly what’s broken - before it breaks worse.

Oladeji Omobolaji
January 24, 2026 AT 07:05Man, I been dealing with this for years. Thought I had IBS till I started bleeding and lost 20 lbs in 3 months. Turned out Crohn’s. Doc said if I’d waited another 6 months, I’d be looking at surgery for sure. Don’t ignore the red flags.
Andrew Smirnykh
January 24, 2026 AT 19:37Interesting breakdown. I’ve seen patients confuse the two all the time in clinic. The real issue isn’t just misdiagnosis-it’s how IBS gets dismissed as "just stress," while IBD gets treated like a crisis. Both are real, but the stigma around IBS makes people suffer in silence.
charley lopez
January 26, 2026 AT 02:58From a clinical gastroenterology standpoint, the fecal calprotectin threshold of 250 µg/g remains the most reliable non-invasive biomarker for distinguishing mucosal inflammation in IBD versus functional disorders. Sensitivity exceeds 90% in active disease states.
Anna Pryde-Smith
January 27, 2026 AT 08:21OMG I HAD THIS. I was told I had IBS for 5 YEARS. Then I collapsed in the bathroom with blood everywhere. ER said "you’re lucky you’re alive." Now I’m on biologics. If you’re bleeding, stop googling and go to a GI. NOW.
Vanessa Barber
January 27, 2026 AT 23:10Wait, so you’re saying IBS isn’t real? That’s rich. My stomach’s been wrecked since college, and I’ve done every test under the sun. Nothing shows up. So I’m just imagining the pain? Cool.
dana torgersen
January 28, 2026 AT 23:48you know… it’s not just about the gut… it’s about the mind… the soul… the energy… the trauma stored in the intestines… i mean… have you ever thought… that maybe… your IBS… is just your spirit screaming for help…? 🌿✨
Dawson Taylor
January 30, 2026 AT 19:10Distinction is essential. Misclassification leads to mismanagement. Functional disorders require neuromodulatory approaches. Inflammatory conditions require immunomodulation. Conflating the two is clinically hazardous.
Kerry Evans
January 31, 2026 AT 20:08Of course you’re going to hear people say "I have IBS" when they mean IBD. Most people don’t know the difference because doctors don’t explain it. And then they get told to "just eat less beans" and call it a day. Pathetic.
Sallie Jane Barnes
February 2, 2026 AT 16:13Thank you for writing this with such clarity. I’ve been in remission from UC for 4 years now, but still get IBS-like symptoms. It’s frustrating when people assume I’m "cured"-but I’m not. I’m managing two conditions at once. This post helped me feel seen.
Laura Rice
February 3, 2026 AT 18:45Y’all… I just found out my cousin has Crohn’s and she’s been telling everyone she has IBS because she didn’t want people to feel bad for her… and now she’s got a fistula and she’s crying because she thought she could just "deal with it"… please… if you’re in pain… get checked… don’t be brave… be smart…