Gout: Understanding Purine Metabolism and How Urate-Lowering Medications Work

What Causes Gout, Really?
You might think gout is just from eating too much steak or drinking beer. But the real story starts inside your cells-with purine metabolism. When your body breaks down purines-found in meat, seafood, and even your own DNA-it produces uric acid. Normally, your kidneys flush it out. But when too much builds up, it forms sharp, needle-like crystals in your joints. That’s when the pain hits: redness, swelling, and a burning sensation so intense even a bedsheet can feel unbearable.
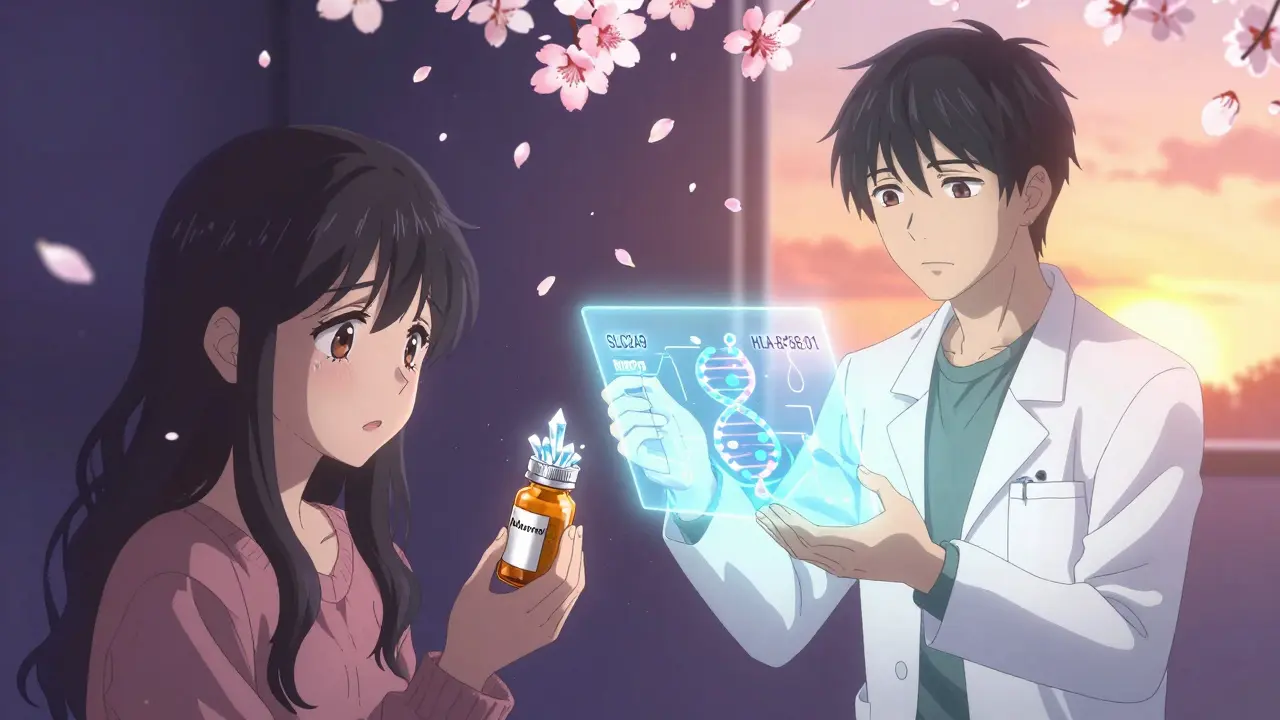
This isn’t just about diet. About 90% of people with gout have trouble excreting uric acid, not making too much of it. Your kidneys reabsorb 90% of the uric acid they filter, thanks to transporters like URAT1 and GLUT9. If those are overactive, uric acid piles up. And if you have a genetic variation in SLC2A9, your body might be wired to hold onto even more.
Scientists found out why humans even have this problem: we lost the enzyme uricase around 15-20 million years ago. Other animals break down uric acid into a harmless compound called allantoin. We don’t. So for us, uric acid is the end of the line-and if it hits 6.8 mg/dL or higher, crystals start forming. That’s the line between normal and gout.
How Urate-Lowering Medications Fix the Problem
There are three main ways to lower uric acid, and each targets a different part of the problem.
Xanthine oxidase inhibitors like allopurinol and febuxostat stop your body from making uric acid in the first place. They block the enzyme xanthine oxidase, which turns xanthine into uric acid. Allopurinol has been around since the 1960s and costs about $4 a month. Febuxostat, approved in 2009, works faster and is stronger-67% of people hit their target levels on 80 mg/day, compared to 47% on allopurinol. But it comes with a black box warning: the CARES trial showed a higher risk of heart-related death in people with existing heart disease.
Uricosurics like probenecid tell your kidneys to dump more uric acid. They block URAT1, the transporter that pulls uric acid back into your blood. Probenecid works well if your kidneys are healthy, but it’s useless if your creatinine clearance is below 50 mL/min. Lesinurad used to be paired with allopurinol to boost results, but it was pulled from the market in 2019 because it damaged kidneys in some patients.
Uricase agents like pegloticase are the nuclear option. They’re not pills-they’re IV infusions given every two weeks. Pegloticase turns uric acid into allantoin, the same harmless waste product other animals make. It works wonders for people with tophi (those visible lumps of crystals under the skin). In clinical trials, 42% of patients saw their tophi shrink or disappear within six months. But it costs over $16,000 a month. And because your body sees it as a foreign protein, 26% of people have serious infusion reactions. You need to be pre-treated with steroids and antihistamines, and you must be tested for HLA-B*58:01, a genetic marker that increases the risk of severe allergic reactions.
Why Most People Fail at Gout Treatment
The biggest mistake? Not taking the meds long enough-or not taking enough of them.
Doctors often start allopurinol at 100 mg a day. That’s too low for most people. The 2020 ACR guidelines say to start low, then increase by 100 mg every 2-5 weeks until your uric acid is below 6.0 mg/dL. For severe gout, aim for 5.0 mg/dL. Most patients need 300 mg or more. Yet a 2024 study found only 29% of primary care doctors ever increase the dose beyond the starting amount.
Dr. Michael Pillinger from NYU says 92% of patients reach target levels when allopurinol is titrated properly. But 61% of people quit their meds within a year. Why? Because when you start lowering uric acid, crystals start to dissolve-and that can trigger flares. Many patients think the medicine isn’t working because they get worse before they get better. That’s why guidelines say to take colchicine (0.6 mg daily) for at least six months when starting treatment. But most patients aren’t told this.
And then there’s cost. Allopurinol is cheap. Febuxostat is 14 times more expensive. Pegloticase? It’s over $197,000 a year. One Reddit user said they needed 17 insurance appeals just to get pegloticase approved. That’s not treatment-it’s a battle.

Diet Matters-But Not Like You Think
Yes, organ meats like liver have 400 mg of purines per 100 grams. Anchovies? 500 mg. Beer? Up to 20 grams of purines per liter. These can raise your uric acid by 1-2 mg/dL. But here’s the catch: even if you go completely meat-free, diet alone rarely drops uric acid enough to prevent flares.
Studies show that dietary changes reduce uric acid by about 1-2 mg/dL on average. If you’re at 9.5 mg/dL, that’s helpful-but not enough. You still need medication. Alcohol, especially beer and spirits, is the worst offender because it blocks uric acid excretion. Wine is less risky. Sugary drinks, especially those with high-fructose corn syrup, are just as bad as alcohol because fructose boosts purine production.
Low-fat dairy, cherries, and coffee might help a little. But they’re not substitutes for treatment. Think of diet as a sidekick, not the hero.
What’s New in Gout Treatment?
The next wave of drugs is already in the pipeline.
Verinurad, a new selective URAT1 inhibitor, is in Phase III trials. When combined with febuxostat, it pushed 74% of patients to target uric acid levels in just 12 weeks. That’s better than any current combo.
Arhalofenate is another promising drug. It doesn’t just lower uric acid-it also reduces inflammation. In a 2024 trial, it cut flare frequency by 58% compared to placebo. That’s huge. Most meds lower uric acid but don’t touch the inflammation cycle.
Researchers are also looking at personalized medicine. If you carry the SLC2A9 variant, you might respond better to uricosurics. If you have the HLA-B*58:01 gene, allopurinol could be dangerous. Genetic testing before starting treatment might become standard.
And there’s talk of longer-lasting uricase shots-maybe once a month instead of every two weeks. That could change everything for people who can’t handle frequent IVs.
What You Should Do Right Now
If you have gout and aren’t on urate-lowering therapy, ask your doctor why. If you’re on allopurinol and still getting flares, ask if your dose is high enough. Most people need 300 mg or more. If you can’t tolerate allopurinol because of a rash, ask about febuxostat-but only if you don’t have heart disease.
Get your uric acid level tested every 2-5 weeks when starting treatment. Don’t wait six months. And if you’re on any of these meds, take colchicine daily for at least six months to prevent flares during the early phase.
And if you’re considering a diet change? Fine. But don’t stop your meds. You’re not fixing this with kale smoothies alone.
Why This Matters Beyond Your Toes
Gout isn’t just a joint problem. It’s a sign of deeper metabolic chaos. Over 65% of gout patients have high blood pressure. Most are overweight. Many have diabetes or kidney disease. Treating gout isn’t just about stopping pain-it’s about preventing heart attacks, strokes, and kidney failure.
The global gout market is growing fast, because the problem is growing. In Asia, cases have exploded. In the U.S., 70% of patients are over 65. With aging populations and diets full of processed foods and sugar, gout isn’t going away.
The good news? We have the tools. We just need to use them right.
