C. diff Colitis: How Antibiotics Trigger It and Why Fecal Transplants Work

When you take an antibiotic for a sinus infection or a urinary tract infection, you expect to feel better. But for some people, that same pill sets off a chain reaction inside their gut that leads to severe diarrhea, cramping, fever, and even life-threatening complications. This isn’t just bad luck-it’s C. diff colitis, a dangerous infection triggered by the very drugs meant to heal you.
How Antibiotics Break Your Gut
Your gut is home to trillions of bacteria, most of them harmless or even helpful. They digest food, train your immune system, and keep bad bugs in check. But when you take certain antibiotics, especially broad-spectrum ones, you don’t just kill the bad bacteria-you wipe out the good ones too. That’s when Clostridioides difficile, or C. diff, gets its chance. C. diff isn’t new. It’s been around for centuries, quietly living in some people’s guts without causing harm. But when antibiotics disrupt the balance, it multiplies fast and releases toxins that attack the colon lining. The result? Watery diarrhea, abdominal pain, fever, and in severe cases, colon swelling, perforation, or sepsis. Not all antibiotics carry the same risk. Research shows some are far more dangerous than others. A 2023 study analyzing over 33,000 hospital stays found that piperacillin-tazobactam, a common IV antibiotic, had the highest risk-more than double the chance of triggering C. diff compared to other drugs. Other high-risk antibiotics include clindamycin, later-generation cephalosporins like ceftriaxone, and fluoroquinolones like ciprofloxacin. On the flip side, tetracyclines like doxycycline are much safer. They’re less likely to wipe out your gut flora, making them a better choice when possible. The CDC says any antibiotic can cause C. diff, but the risk climbs with every extra day you’re on it. After 14 days, the danger spikes again. That’s why doctors are now told to review antibiotics every 48 to 72 hours and stop them as soon as they’re no longer needed.The Hidden Risk: Asymptomatic Carriers
Not everyone who gets C. diff had recent antibiotics. Some people carry the bacteria without symptoms-they’re silent carriers. A 2024 study found these individuals have a 27 times higher risk of developing full-blown C. diff colitis, even without antibiotics. That’s scary because they can spread it to others in hospitals or nursing homes without knowing it. But here’s the twist: for these carriers, antibiotics don’t make the risk much worse. Their gut is already primed for trouble. For everyone else, though, antibiotics are the main trigger. That’s why stopping unnecessary antibiotics is the single most effective way to prevent C. diff. Hospitals that cut down on broad-spectrum drugs have seen infection rates drop by 20% or more.When Standard Treatment Fails
The go-to treatment for C. diff has long been vancomycin or fidaxomicin-oral antibiotics that target the bacteria. But here’s the problem: up to 30% of patients get it back after treatment. And each recurrence makes the next one more likely. After two or three episodes, the odds of another flare-up jump to 60%. That’s where things get desperate. People end up in the hospital again and again. Some lose weight, get weak, and can’t work. One Reddit user described going through five relapses over two years-each time treated with vancomycin, each time coming back worse. He finally found relief only after a fecal transplant.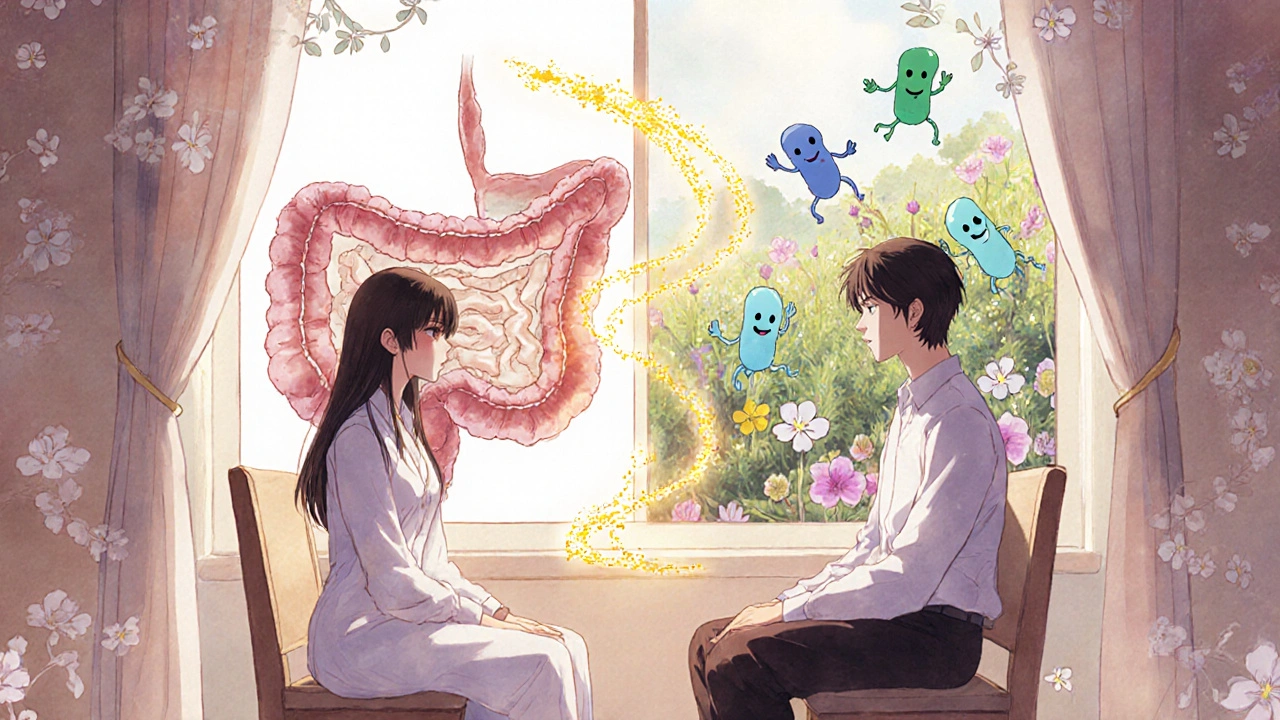
Fecal Transplant: The Unexpected Cure
Fecal microbiota transplantation (FMT) sounds gross, but it’s one of the most effective treatments in modern medicine. The idea is simple: take healthy stool from a screened donor, process it, and put it into the patient’s colon. This restores the good bacteria that antibiotics destroyed. A landmark 2013 study in the New England Journal of Medicine showed FMT cured 94% of patients with recurrent C. diff after just one or two treatments. Compare that to vancomycin, which worked in only 31% of cases. Since then, multiple studies have confirmed similar results-85% to 90% success rates for people who’ve had three or more recurrences. Today, FMT isn’t just a last-resort trick done in a lab. The FDA has approved two standardized products: Rebyota and Vonjo. These are oral capsules or enemas made from carefully tested donor stool. They’re safer, more consistent, and easier to deliver than old-school colonoscopies. Delivery methods vary. About 65% of FMTs are done via colonoscopy. Another 20% use enemas. The rest use capsules you swallow-no procedure needed. Costs range from $1,500 to $3,000, which is far less than the $11,000 average cost of a single hospital stay for recurrent C. diff.Why FMT Works Better Than More Antibiotics
Antibiotics treat the infection, but they don’t fix the broken ecosystem. FMT fixes the root cause: a missing microbiome. It’s like reseeding a lawn after you’ve sprayed it with herbicide. You don’t just kill the weeds-you plant new grass so they can’t grow back. That’s why patients who get FMT rarely relapse. Their gut gets its natural defenses back. Some doctors now recommend FMT after just two recurrences, not three, because the damage keeps piling up. The American Gastroenterological Association updated its guidelines in 2021 to reflect this. There are risks, of course. A few cases of serious infections have been linked to FMT when donor stool wasn’t screened well enough. That’s why all approved products now come from donors tested for over 50 pathogens, including HIV, hepatitis, and drug-resistant bacteria. Long-term effects are still being studied, but so far, no major issues have appeared in follow-ups of 5+ years.
What’s Next? Beyond the Poop
Scientists aren’t stopping at FMT. They’re working on targeted therapies that deliver only the good bacteria-no stool needed. One such product, SER-109, is a pill made from purified spores of healthy gut bacteria. In a 2022 trial, it cured 88% of patients with recurrent C. diff, matching FMT’s success. Another promising option is bezlotoxumab, a monoclonal antibody that neutralizes one of C. diff’s toxins. When given with antibiotics, it cuts recurrence rates by 10%. It’s expensive-around $3,700 per dose-but it’s an option for people who can’t or won’t get FMT. The CDC now calls C. diff an “urgent threat.” It causes 500,000 infections and nearly 30,000 deaths every year in the U.S. alone. The total cost? Over $6 billion. But progress is happening. Hospitals with strong antibiotic stewardship programs have cut infection rates by up to 40%. And with new microbiome therapies approved in 2022 and 2023, the future looks brighter.What You Can Do
If you’re prescribed an antibiotic, ask:- Is this really necessary?
- Is there a narrower-spectrum option?
- Can I take it for fewer days?
Can C. diff go away without treatment?
In mild cases, especially if the triggering antibiotic is stopped right away, some people recover on their own. Their gut bacteria naturally bounce back. But if symptoms last more than a few days or include fever, blood in stool, or severe pain, medical treatment is needed. Waiting too long can lead to dangerous complications.
Are probiotics helpful for C. diff?
The evidence is mixed. Some studies show certain probiotics, like Saccharomyces boulardii, might reduce recurrence slightly. But the Infectious Diseases Society of America says there’s not enough proof to recommend them for prevention. Worse, in people with weakened immune systems, probiotics can cause dangerous infections. Don’t rely on them alone.
Is FMT safe for older adults?
Yes. Most FMT patients are over 65, and studies show it’s just as effective and safe in older adults as in younger people. In fact, since older adults are at higher risk for severe C. diff, FMT is often recommended for them after just two recurrences. Don’t assume age makes it too risky-talk to your doctor.
How long does it take to feel better after FMT?
Many patients see improvement within 24 to 48 hours. Diarrhea stops, energy returns, and abdominal pain fades. Full recovery of gut balance takes a few weeks, but most people report feeling like themselves again within a week. The key is that relapse rates drop dramatically after FMT-unlike with antibiotics.
Can I get C. diff from eating contaminated food?
It’s possible, but rare. C. diff spores are found in soil, water, and animal feces, and they can contaminate food. But infection usually only happens if you already have a disrupted gut microbiome-usually from recent antibiotics. Healthy people rarely get sick from eating contaminated food. The biggest risk is person-to-person spread in hospitals or nursing homes, especially if hygiene is poor.
Will I need a colonoscopy for FMT?
Not anymore. While colonoscopy was once the standard method, most FMTs today are done with oral capsules or enemas. Capsules are the easiest-just swallow them with water. Enemas are done at home or in a clinic. Colonoscopy is still used in some cases, especially if the patient has other colon issues, but it’s no longer the default.

Tina Dinh
November 29, 2025 AT 13:29linda wood
November 29, 2025 AT 16:38LINDA PUSPITASARI
November 30, 2025 AT 23:59gerardo beaudoin
December 1, 2025 AT 13:48Joy Aniekwe
December 2, 2025 AT 00:14Latika Gupta
December 2, 2025 AT 18:13Sohini Majumder
December 3, 2025 AT 08:10tushar makwana
December 3, 2025 AT 21:58Peter Axelberg
December 3, 2025 AT 22:52Monica Lindsey
December 5, 2025 AT 07:52