Bladder Infection Prevention Plan: A Step‑by‑Step Guide
Personalized Bladder Infection Prevention Plan Builder
Your Personalized Prevention Plan
Answer these questions to generate your custom bladder infection prevention plan.
Recommended Prevention Actions
When it comes to staying healthy, bladder infection prevention plan is a structured set of habits and interventions designed to lower the risk of urinary tract infections (UTIs). Whether you’ve dealt with a one‑off infection or have recurring episodes, a plan gives you clear actions instead of vague advice.
Why Bladder Infections Happen
Most bladder infections start when bacteria travel up the urethra and multiply in the bladder. The most common culprit is Escherichia coli (E. coli), a gut bacterium that can hitch a ride on the skin around the genital area. Other contributors include Staphylococcus saprophyticus and, in catheter‑using patients, Pseudomonas aeruginosa. Once inside the bladder, these microbes trigger inflammation, leading to the classic symptoms of burning on urination, urgency, and cloudy urine.
Assess Your Personal Risk
Before you build a plan, know which factors apply to you. Common risk factors include:
- Female anatomy - a shorter urethra makes bacteria travel faster.
- Sexual activity - intercourse can push bacteria toward the urethra.
- Hormonal changes - post‑menopausal estrogen loss thins the urinary tract lining.
- Diabetes - high blood sugar feeds bacteria and impairs immune response.
- Catheter use - provides a direct pathway for microbes.
- Previous UTIs - scar tissue can make future infections easier.
Write down the items that match your lifestyle; they’ll guide how aggressive your plan needs to be.
Core Daily Habits
These habits form the backbone of any effective bladder infection prevention plan.
- Stay hydrated - aim for at least 2 liters (about eight 8‑oz glasses) of water daily. Frequent urine flow flushes bacteria before they settle.
- Urinate when the urge hits - holding urine encourages bacterial growth.
- Empty your bladder fully - try a two‑minute pause after finishing to allow residual urine to drain.
- Practice proper wiping - always front‑to‑back for women; men should keep the area clean and dry.
- Avoid irritating products - scented soaps or feminine sprays can disrupt the natural flora.

Dietary Support: Probiotics, Cranberries, and More
Food can boost the urinary tract’s defenses.
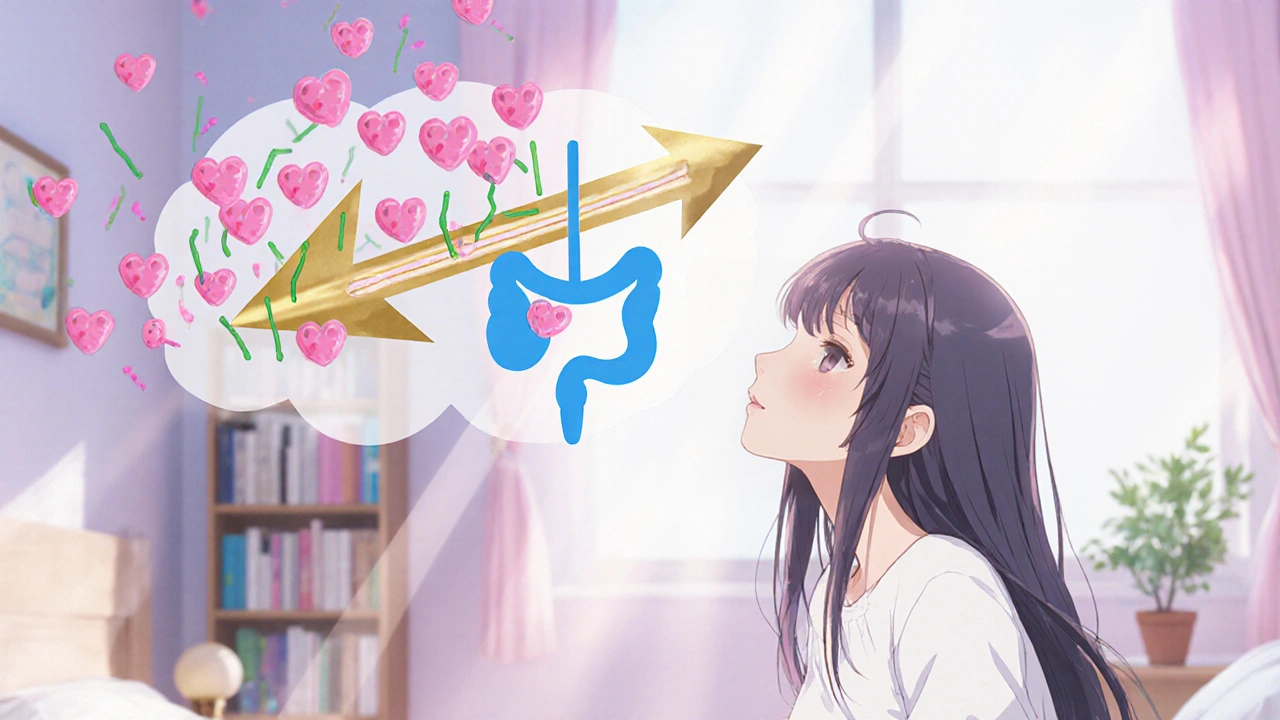
Probiotics containing Lactobacillus species help maintain a healthy vaginal microbiome, making it harder for E. coli to colonize. Look for daily doses of at least 1 billion CFU in fermented foods (yogurt, kefir, sauerkraut) or a quality supplement.
Cranberry extract contains proanthocyanidins (PACs) that stop bacteria from sticking to bladder walls. Clinical trials show a daily 300 mg dose reduces recurrent UTI risk by about 30 %.
Vitamin C increases urine acidity, creating a less friendly environment for bacteria. A modest 500 mg supplement can be useful, especially when combined with the other strategies.
Medical Strategies for High‑Risk Individuals
If you fall into any high‑risk categories (catheter use, post‑menopausal, diabetes), consider talking to a clinician about these options.
- Low‑dose prophylactic antibiotics taken after intercourse or daily can break the infection cycle, but they should be used sparingly to avoid resistance.
- Topical estrogen therapy restores the urinary tract lining in post‑menopausal women, lowering recurrence rates by up to 40 %.
- For patients with frequent catheter changes, Silver‑coated catheters reduce bacterial colonization compared with standard silicone tubes.
Vaccines targeting uropathogenic E. coli are under trial; keep an eye on FDA updates, as they could become a future preventive tool.
Special Situations: Pregnancy, Diabetes, and Catheters
Pregnant women experience hormonal shifts that increase urinary stasis. Drinking extra water (up to 3 liters if tolerated) and regular prenatal check‑ups are crucial. Diabetes management should focus on keeping blood glucose under 130 mg/dL fasting; tighter control reduces bacterial growth in urine.
People who require long‑term catheterization should follow a strict catheter‑care protocol: clean technique, regular replacement (every 2-4 weeks depending on material), and routine urine cultures.
Build Your Personal Bladder Infection Prevention Plan
Take the risk factors you identified and match them with the actions above. Use the checklist below to turn vague ideas into daily habits.
- Water intake goal (e.g., 2 L/day)
- Morning and evening bathroom schedule
- Probiotic source (food vs supplement)
- Cranberry dose (300 mg extract)
- Hygiene routine (wipe direction, soap type)
- Medical follow‑up (e.g., discuss estrogen therapy)
- Special considerations (catheter change date, diabetes log)
Review the checklist weekly for the first month, then monthly. Adjust as needed-if you notice any new symptoms, revisit the risk‑factor list.
Quick Reference Table
| Risk Factor | Targeted Action | Frequency / Dose |
|---|---|---|
| Low fluid intake | Increase water consumption | ≥2 L/day |
| Frequent sexual activity | Urinate within 30 minutes after intercourse | Every time |
| Post‑menopausal | Topical estrogen or vaginal moisturizer | As prescribed |
| Diabetes | Maintain HbA1c <7 % and stay hydrated | Continuous |
| Catheter use | Silver‑coated catheters & clean technique | Replace every 2‑4 weeks |
| History of recurrent UTIs | Probiotic + cranberry supplement | Daily |
Frequently Asked Questions
How much water should I drink to prevent a bladder infection?
Aim for at least 2 liters (about eight 8‑oz glasses) a day, more if you’re active or live in a hot climate.
Can cranberry juice really stop UTIs?
Pure cranberry juice contains the active PACs, but most commercial juices are sweetened and diluted. A standardized cranberry extract (300 mg PACs) taken daily is more reliable.
Are probiotics safe for men?
Yes. Lactobacillus‑based probiotics support a balanced gut and genital flora in both sexes and have no known harmful side effects.
When should I see a doctor for a suspected bladder infection?
If you have fever, flank pain, blood in urine, or symptoms lasting longer than 48 hours, seek medical care promptly.
Does estrogen therapy work for everyone?
It’s most effective for post‑menopausal women with recurrent UTIs who have low estrogen levels. A doctor will assess benefits versus risks.
By turning these evidence‑backed steps into a daily routine, you turn the vague idea of ‘staying healthy’ into a concrete bladder infection prevention plan you can stick to.

erica fenty
October 21, 2025 AT 17:04Hydration, urine output, and bacterial load are the three pivotal vectors in any prophylactic protocol, and you’ve captured them succinctly; the checklist format translates complex epidemiology into actionable daily tasks, which is precisely the translational medicine we need, especially for at‑risk cohorts.
Xavier Lusky
October 22, 2025 AT 20:50Never forget that the “natural” cranberry extracts are heavily subsidized by conglomerates seeking market dominance; the push for PAC‑rich supplements conveniently sidelines cheaper, proven interventions like basic hygiene, suggesting an ulterior commercial agenda.
Ashok Kumar
October 24, 2025 AT 00:37Sure, low‑dose antibiotics sound like a quick fix, but the looming resistance crisis makes it a classic case of short‑term relief turning into long‑term regret-perhaps better to focus on diet and fluid intake.
Jasmina Redzepovic
October 25, 2025 AT 04:24From a policy standpoint, the United States has already codified optimal fluid intake guidelines; aligning personal plans with those federal benchmarks ensures compliance, and any deviation risks legal liability under existing health regulations.
Esther Olabisi
October 26, 2025 AT 07:10Totally agree, the checklist is a solid foundation 😃! Adding a quick reminder to swap scented soaps for fragrance‑free options can make a huge difference, especially for those with sensitive microbiomes.
Ivan Laney
October 27, 2025 AT 10:57Let me elaborate on why a comprehensive bladder infection prevention plan must be viewed through a multi‑dimensional lens, integrating physiological, behavioral, and sociocultural components. First, the basic premise that increased fluid intake dilutes urinary solutes is well‑established, yet many patients underestimate the volume required to achieve therapeutic diuresis. Second, urinary stasis, often caused by delayed voiding, directly correlates with bacterial colonization, thus the recommendation to void at the first urge cannot be overstated. Third, the role of the vaginal microbiome, dominated by Lactobacillus, acts as a biological barrier against uropathogenic E. coli; probiotic supplementation therefore supports this defense. Fourth, dietary elements such as cranberry proanthocyanidins interfere with bacterial adhesion, but dosage consistency remains a challenge due to product variability. Fifth, hormonal fluctuations in post‑menopausal women diminish urothelial integrity, making topical estrogen a clinically validated adjunct. Sixth, diabetes management is not merely about glucose control but also about mitigating glucosuria, which provides a nutrient‑rich medium for microbes. Seventh, catheter‑related infections require strict aseptic technique plus periodic replacement schedules, as biofilm formation is a primary driver of resistance. Eighth, the emerging field of uropathogenic vaccine development holds promise, yet regulatory hurdles delay widespread adoption. Ninth, psychosocial factors, including stress and health literacy, influence adherence to daily regimens; patient education must be tailored accordingly. Tenth, antibiotic stewardship is essential; prophylactic regimens should be reserved for high‑risk cases to prevent resistance escalation. Eleventh, regular monitoring through urine cultures can detect asymptomatic bacteriuria early, allowing preemptive adjustments. Twelfth, integration of mobile health reminders can improve compliance with fluid and voiding schedules. Thirteenth, interdisciplinary collaboration among urologists, nutritionists, and primary care providers ensures a holistic approach. Fourteenth, insurance coverage policies can either facilitate or hinder access to supplements and topical therapies, underscoring the need for advocacy. Finally, continuous quality improvement cycles-reviewing outcomes quarterly-enable iterative refinement of the prevention plan, ensuring it remains evidence‑based and patient‑centered.
Vivian Annastasia
October 28, 2025 AT 14:44Oh great, another “quick fix” that will definitely solve everything.
John Price
October 29, 2025 AT 18:30Solid points, especially the reminder to actually finish the pee.