Anticholinergic Burden with Tricyclic Antidepressants: Cognitive and Cardiac Risks

Anticholinergic Burden Calculator
Anticholinergic Burden Calculator
Calculate your total anticholinergic burden score from medications to assess cognitive and cardiac risks. Enter your medications to see their ACB scores and total risk.
Current Medications
Total Anticholinergic Burden Score
0
Recommended Alternatives
How to Interpret Your Score
- 0Minimal risk
- 1-2Low to moderate risk
- 3+High risk (requires review)
When you take a tricyclic antidepressant like amitriptyline or nortriptyline for depression or chronic pain, you might not realize you’re also loading your body with a hidden risk-one that can quietly damage your brain and heart over time. This isn’t speculation. It’s backed by decades of research and now built into clinical guidelines across the UK, US, and beyond. The issue is called anticholinergic burden, and it’s one of the most underrecognized dangers in modern prescribing.
What Is Anticholinergic Burden?
Your brain and body rely on a chemical called acetylcholine to help with memory, attention, digestion, heart rhythm, and even bladder control. Anticholinergic drugs block this chemical. Tricyclic antidepressants (TCAs) are among the strongest blockers out there. They were designed to boost serotonin and norepinephrine to lift mood, but in doing so, they also slam shut acetylcholine receptors like a door you didn’t know was open. The Anticholinergic Cognitive Burden (ACB) Scale measures this effect. TCAs like amitriptyline and nortriptyline get the highest score: 3. That means “definite high anticholinergic activity.” Compare that to SSRIs like sertraline or escitalopram, which score 0 or 1. Even over-the-counter sleep aids like diphenhydramine (Benadryl) or allergy pills like chlorphenamine carry a score of 2 or 3. When you stack these together-TCA plus sleep aid plus bladder medication-you’re not just adding side effects. You’re building up a dangerous cumulative load.How TCAs Affect Your Brain
One of the most alarming findings came from a 7-year study of over 3,400 adults over 65, published in JAMA Internal Medicine. People taking medications with an ACB score of 3 or higher had a 54% higher risk of developing dementia. And it wasn’t just correlation. When researchers looked closer, TCAs were the biggest contributors. Even after people stopped taking the drugs, the cognitive damage didn’t always reverse. Clinicians see this in real time. Patients come in with memory lapses, confusion, trouble finding words. Families assume it’s early dementia. But after switching off the TCA, their thinking clears up within weeks. One Reddit thread from a psychiatrist described a 72-year-old man who couldn’t remember his grandchildren’s names. He was on amitriptyline for neuropathic pain. After tapering off, his MMSE score jumped from 21 to 27 in three months. He was never demented-he was drugged. The problem? These symptoms look exactly like Alzheimer’s. That’s why NICE guidelines now say: if someone is showing signs of cognitive decline, check their medication list first. Rule out anticholinergic burden before labeling it dementia. It’s not just a side effect. It’s a mimic.How TCAs Threaten Your Heart
Your heart doesn’t just pump blood-it relies on precise electrical signals to keep rhythm. TCAs interfere with those signals. They act like Class 1A antiarrhythmics, but without the safety controls. Amitriptyline can prolong the QT interval by 20-30% at standard doses. In overdose, that number can spike to 50%. That’s not theoretical. Emergency rooms see this every day. Studies show TCAs carry about three times the risk of dangerous arrhythmias compared to SSRIs. Amitriptyline specifically is linked to a 2.8 times higher risk of QT prolongation than sertraline. For someone with existing heart disease, high blood pressure, or an electrolyte imbalance, this is a ticking bomb. One patient in the Mended Hearts forum described palpitations and dizziness after just three weeks on amitriptyline. An ER visit revealed a prolonged QT interval. He was lucky-no cardiac arrest. But many aren’t. The FDA and the Beers Criteria have flagged TCAs as potentially inappropriate for adults over 65 since 2012. The 2023 update made it stronger: avoid them unless every other option has failed. That’s not a suggestion. It’s a warning.
Why Are TCAs Still Prescribed?
If the risks are this clear, why do doctors still write these scripts? Because for some people, they work-better than anything else. TCAs are still the most effective option for treatment-resistant depression. They’re also first-line for certain types of nerve pain, especially diabetic neuropathy or fibromyalgia. For patients who’ve tried SSRIs, SNRIs, gabapentin, and even opioids with no relief, TCAs can be a lifeline. But here’s the catch: that’s a small group. Most people with depression or mild-to-moderate pain don’t need them. Yet, outdated habits persist. Older doctors trained in the 80s and 90s still default to amitriptyline. Pharmacies stock it because it’s cheap. Insurance often covers it before newer drugs. And patients don’t ask questions-they just take what’s handed to them.What Should You Do Instead?
The good news? There are safer, equally effective alternatives. For depression: SNRIs like duloxetine or venlafaxine. They work nearly as well as TCAs but have ACB scores of 0 or 1. SSRIs like escitalopram are even safer. For nerve pain: gabapentin, pregabalin, or even topical lidocaine patches. Cognitive behavioral therapy (CBT) has strong evidence for both depression and chronic pain, with zero anticholinergic risk. If you’re on a TCA and doing well, don’t panic. But do ask your doctor: “Is this still the best option for me?” and “What’s my total ACB score?” Most electronic health records now include ACB calculators. If yours doesn’t, ask for one. You can even use free online tools like the ACB Calculator from bpacnz.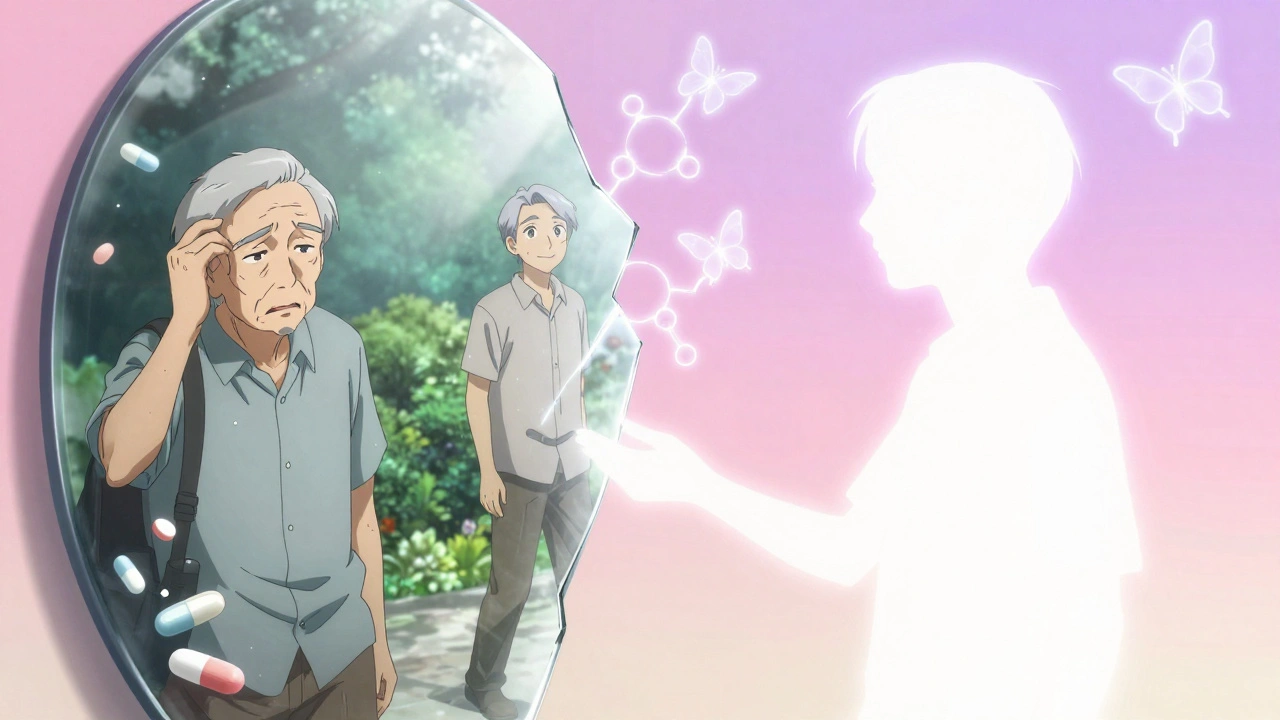

Rob Purvis
December 12, 2025 AT 11:35Wow, this is one of the most important posts I’ve read this year-seriously. I had no idea TCAs had an ACB score of 3. My dad’s been on nortriptyline for 12 years for sciatica, and he’s been forgetting where he put his keys, then his wallet, then his own birthday… I just thought it was aging. Now I’m scheduling a med review tomorrow. Thank you for the clarity.
Levi Cooper
December 13, 2025 AT 18:32Of course the medical establishment is pushing SSRIs now-because Big Pharma doesn’t make money off cheap generics. Amitriptyline’s been saving people for 60 years. If you can’t handle a little dry mouth and fuzzy thinking, maybe you shouldn’t be on meds at all. This is just another example of over-medicalizing normal aging.
Ashley Skipp
December 15, 2025 AT 17:39My GP just switched me from amitriptyline to venlafaxine last month after I mentioned my brain fog. Within two weeks I remembered my husband’s anniversary. I cried. No joke. This isn’t theoretical. It’s real life.
Nathan Fatal
December 16, 2025 AT 08:26The anticholinergic burden isn’t just about cognition-it’s a systemic burden. Acetylcholine regulates parasympathetic tone, so blocking it affects GI motility, urinary retention, pupillary dilation, and cardiac conduction. The JAMA study is solid, but the real issue is that clinicians still treat symptoms in isolation. You don’t just treat depression-you treat the whole pharmacological ecosystem. The Beers Criteria aren’t suggestions-they’re ethical obligations. And if your EHR doesn’t flag ACB scores, demand a better system. This isn’t niche-it’s foundational pharmacology.
nikki yamashita
December 17, 2025 AT 15:14Just switched off amitriptyline after 8 months. My energy came back. My memory came back. I started remembering dreams again. Who knew a pill could make you feel like a ghost? I’m so glad I listened to my gut. You’re not weak for asking for alternatives-you’re smart.
Laura Weemering
December 18, 2025 AT 02:06Have you ever considered that the dementia link might be reverse causality? People with early neurodegeneration are more likely to be prescribed TCAs for depression or insomnia-so the drug isn’t causing it, it’s just a marker. And what about the placebo effect in deprescribing studies? The cognitive ‘improvement’ could just be expectation bias. Also-did you know that SSRIs increase bleeding risk and sexual dysfunction? Are we just swapping one poison for another? The system is broken.
Stacy Foster
December 18, 2025 AT 04:54THIS IS A GOVERNMENT PLOT. TCAs are being phased out because they’re too cheap. The FDA, WHO, and Big Pharma are all in bed together to push expensive brand-name SSRIs. They don’t want you to know that a 10-cent pill can do the same job. Your ‘ACB calculator’? It’s a scam. Your doctor’s ‘guidelines’? Propaganda. My uncle took amitriptyline for 30 years and lived to 92. He never had dementia. They’re lying to you.
Reshma Sinha
December 19, 2025 AT 12:20As a clinical pharmacist in Mumbai, I’ve seen this firsthand. Elderly patients on multiple anticholinergics-TCA + diphenhydramine + oxybutynin-are presenting with delirium. We’ve started screening all geriatric patients for ACB score. It’s changed practice. But awareness is still low. We need more education, not just guidelines. And yes, SSRIs aren’t perfect-but they’re safer. We’re not rejecting TCAs-we’re refining our choices.
Lawrence Armstrong
December 21, 2025 AT 12:11Just wanted to add-when tapering, go slow. I went from 75mg to 50mg over 3 weeks, then 25mg over 4 weeks. No withdrawal. Also, if you’re switching to an SNRI, monitor BP-venlafaxine can spike it. And if you’re on a TCA for pain, consider topical capsaicin or TENS. I’ve seen people get just as much relief without the brain fog. 🙏