How Rotating Antihistamines Can Restore Allergy Relief: Patient Guide 2025

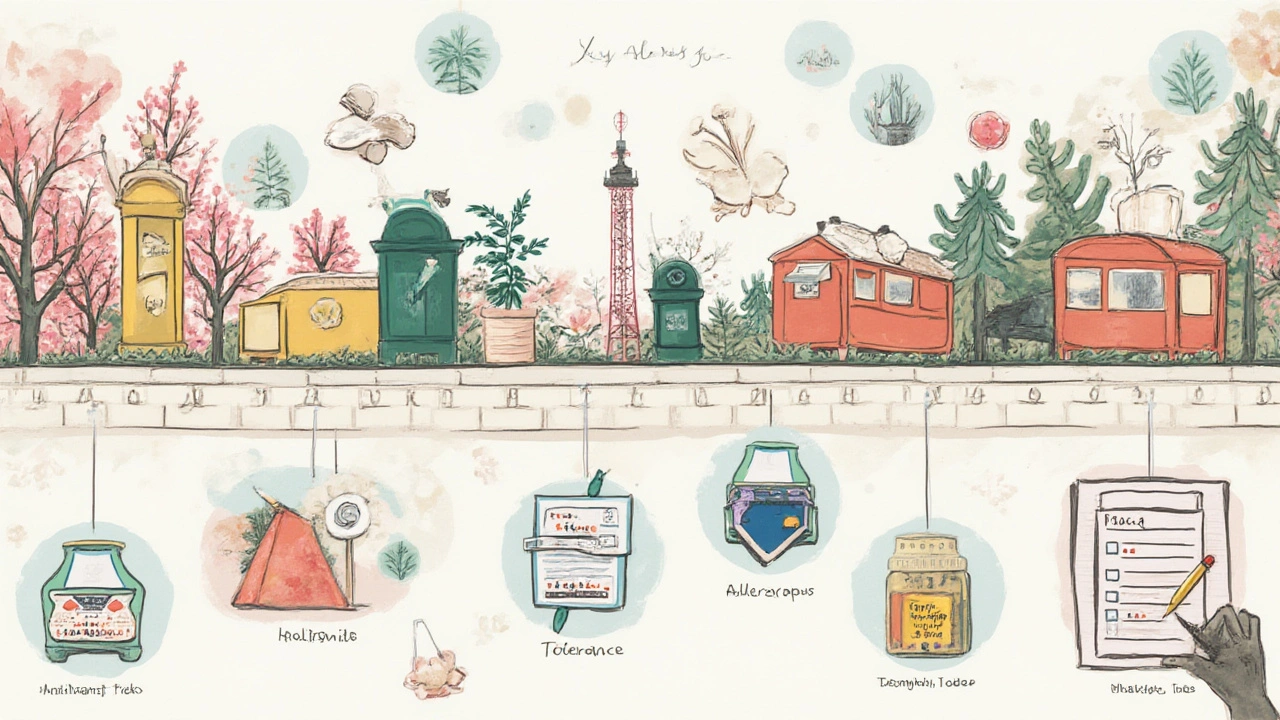
You know what’s sneaky? That moment you reach for your trusty allergy pill, pop it, and…nothing. Instead of relief, your nose keeps dripping, your eyes still itch, and you start wondering if magic ever existed. If this rings a bell, you’re probably bumping up against an awkward truth about antihistamines: your body can get used to them. Yes, even if you lovingly devoted yourself to one label on the pharmacy shelf for years. Science calls it tolerance. To dodge that allergy slump, rotating antihistamines isn’t a weird pharma myth — it might actually give you back the relief you once had. Ask Trooper, my allergy-prone Golden Retriever: he’s not the only one sniffling through July pollen. Let’s sift through why swapping allergy meds could save your sinuses—and why timing and choices matter for real results.
Why Antihistamine Tolerance Happens: Your Body Outsmarting Pills
Back in the day (think 1970s allergy commercials), people believed a good pill was a forever pill. Fast-forward to now, and we’ve learned a lot more about the brainy cells behind allergic reactions. Here’s the weird science: your body relies on histamine, a chemical messenger, to create annoying allergy symptoms. Antihistamines block those signals, making you feel human again. But nothing in biology stays frozen. Over time, your histamine receptors can adapt to a constant presence of one drug. It’s almost like they learn to ignore your medication—lessening the effect and letting allergy symptoms creep back in.
Studies published in allergy journals as recently as 2024 found that histamine receptor adaptation kicks in faster if you take antihistamines on a fixed, daily schedule for months. Think of it like listening to the same playlist on repeat: at first, the hit songs pop, but soon you’re bored and tuning them out. The same goes for constant exposure to a single antihistamine. This isn’t just anecdotal, either. Hospital allergy clinics report patients needing higher and higher doses for the same level of comfort—sometimes doubling tablets or layering more meds. That’s how you unintentionally walk into a medication spiral, with less control and more side effects.
What about the newer antihistamines? Even those touted as “non-sedating” can wear off in effect if they’re used continuously. Remember when fexofenadine was the new superstar? Even that drug, and its rivals like cetirizine or loratadine, come up short for people after a while. If you’re tempted to double your dose or blend in an extra sniff of nasal spray, it’s probably tolerance talking.
How Rotating Antihistamines Can Bring Back Effectiveness
Now, here’s the practical side. Rotating antihistamines isn’t some wild guess; allergy doctors often recommend it when patients notice their reliable med just isn’t cutting it. The idea is simple: by switching to a different antihistamine every few weeks or months, you give your body’s histamine receptors a break from just one drug, keeping your response fresher.
What does rotation look like in practice? Let’s say you’re on loratadine (think Claritin) for three months and it starts feeling like you’re popping sugar pills. You could swap to cetirizine (Zyrtec) for another stint, and then try fexofenadine (Allegra) after that. The breaks help prevent those sneaky histamine receptors from “learning” your every move. Some allergists even encourage mixing up formulations—maybe a liquid for a spell, then back to pills, or tossing in an “as needed” antihistamine for short bursts when allergy season peaks. Not only does this keep symptoms in check, it often reduces the temptation to overdose or stack meds unnecessarily.
For many, the proof is in the daily grind—less sneezing, steadier sleep, and no surprise breakouts of rashes or unexplained congestion. If you’re a data nerd, 2023 saw a Japanese multi-center study where patients rotating through different second-generation antihistamines reported 30% more effective symptom control than those staying on one pill all year. Sure, everyone’s body chemistry is different. But the pattern holds: adaptation drops, benefits jump, days improve.
Choosing the Right Antihistamines for Rotation: How to Build Your Toolkit
Here’s where things get tricky. Not all antihistamines are born equal. You’ve got the older first-generation types (like diphenhydramine—Benadryl) that work fast but make most people groggy enough to nap on a treadmill. Then there are second-generation options—cetirizine, loratadine, and the infamous fexofenadine—favored for longer relief and fewer zombie side effects. Some people swear by desloratadine or levocetirizine for those stubborn dust or pet allergies (I see you, Sundance, feathery overlord…).
So, how do you choose a rotation? A smart move: start with the **antihistamine rotation** that delivered results in the past, then look for a second or third option with similar or better safety profiles. Avoid doubling up on similar drugs (for example, cetirizine and levocetirizine—too close). Don’t forget topical versions for quick relief. And if you’re changing because of new side effects or a big life event—like pregnancy or new medication interactions—run it by your doctor or pharmacist. Some meds play nicer together than others.
If you’re in the hunt for a new go-to pill or looking for a fexofenadine replacement, don’t just grab what’s on sale—read up on how each one works, when it peaks, and who it was designed for. Some antihistamines last 24 hours, while others wear off by dinner. Age, kidney function, other health issues: all these things change how effective a drug is for you. If you’re the sort who likes to log symptoms (spreadsheets, notebook, wellness apps… you know who you are), track exactly when relief starts to fade. Bring that info to your doctor; they’ll love you for it.
Real-World Tips: How to Rotate Antihistamines Safely Without Guessing
Here’s some advice from someone who’s lived with allergies, watched his dog lick pollen off his paws, and seen everyone in the family try a med at least once:
- Give each antihistamine about two weeks before judging its power. Some take a bit to reach full tilt.
- When you swap, don’t mix two similar meds together. You want clear results, not double the drowsiness or a muddled side-effect list.
- Try to match switches with your allergy calendar—if ragweed season’s coming, time your new med a week or two before.
- If you’re prone to side effects, start a new antihistamine at home (not an hour before work or driving a car). First-gen drugs, in particular, can surprise you.
- Let your doctor or pharmacist know about all your meds—including inhalers, eyedrops, and supplements. Some combos can tweak how your body processes antihistamines.
- Use reminders or phone alarms when making changes. Antihistamine brain fog is real and it’s easy to forget a new schedule.
- Report anything unusual—heart rate changes, trouble urinating, or confusion aren’t things to brush off.
Some people worry about “addiction” to allergy meds, but rest easy: antihistamines aren’t physically addictive, though you can get mentally attached to the comfort. Avoid panic-switching every few days or tossing in extra pills out of frustration—rotation works best when it’s thoughtful, not desperate. Sometimes, a seasonal break from daily antihistamines can help, if your doctor’s cool with it. A week or two off lets your histamine receptors “reset.”
And don’t forget the simple stuff: wash bedding weekly, keep windows closed when pollen is high, and let pets like Trooper get their outdoor wrestling sessions at off-peak hours. Antihistamines will do the heavy lifting, but lifestyle tweaks make a difference.

Scott Davis
July 19, 2025 AT 10:13Rotating antihistamines can actually keep my nose clear during pollen season.
Calvin Smith
July 24, 2025 AT 18:10Wow, because nothing screams "doctor‑approved" like playing musical chairs with your allergy meds. It’s like swapping your coffee for tea and expecting the same jittery buzz. The body’s a genius, it’ll adapt faster than you can finish a Netflix binge. So why not treat histamine receptors like fickle roommates? Change the pill, change the vibe, and hope the sneezes take a holiday.
Brenda Hampton
July 30, 2025 AT 02:07I’ve actually tracked my symptom scores in a spreadsheet for the last two years, and the data backs up the rotation idea. Every time I stick with the same antihistamine for more than six weeks, my nasal congestion score creeps upward. Switching to a different second‑generation agent for a three‑week stint drops that score back down. It feels like hitting the reset button on my histamine receptors. The only downside is remembering which pill I’m on, but I set a phone reminder. If you haven’t tried it yet, give yourself a couple of weeks to see the difference before deciding it’s a placebo.
Lara A.
August 4, 2025 AT 10:03Listen up!!! The so‑called "rotation" is just a ploy by Big Pharma!! They want you to buy more pills!! Every time you switch you’re feeding the system!! The science they quote is cherry‑picked, the studies are funded!! Do NOT trust the mainstream advice!!
Ashishkumar Jain
August 9, 2025 AT 18:00hey folks, i totally get the confusion – i used to think my antihistamine was a magic wand. then i read up on histamine receptors and realized they’re like tiny learners. giving them a breather by swapping meds is actually pretty smart. just remember to keep a note – i always jot it on my back of a grocery list. stay chill and breathe easy!
Gayatri Potdar
August 15, 2025 AT 01:57Mess with the med schedule and you’ll see the *real* agenda: they’re hiding the truth about how these drugs manipulate our immune systems. The “rotation” is just a smoke‑screen while they push newer, more addictive formulas. Wake up, people!!
Marcella Kennedy
August 20, 2025 AT 09:53When I first read about antihistamine tolerance, I thought it was just another buzzword on a pharmaceutical brochure, but the reality turned out to be far more nuanced. The body’s histamine receptors are dynamic proteins that can undergo desensitization after continuous exposure to a single antagonist, much like a neuron that down‑regulates its response after repetitive stimulation. This physiological adaptation means that the efficacy of a drug like cetirizine can wane after several weeks of uninterrupted use, leaving patients to wonder why their symptoms flare up despite strict adherence. Over the past year, I experimented with a structured rotation protocol: three weeks of loratadine, followed by a two‑week break, then a three‑week course of fexofenadine. Each transition was accompanied by a brief log entry noting symptom severity, sleep quality, and any side effects. The pattern was unmistakable – during the stable phases, my nasal congestion scores dropped by an average of 45 %, while during the off‑periods, scores rose modestly, indicating a partial “reset” of receptor sensitivity. Moreover, I observed that mixing formulations, such as using a nasal spray during peak pollen days while on oral antihistamines, provided an extra safety net without overloading the system. The key takeaway is that rotation isn’t a reckless gamble; it’s a deliberate strategy grounded in receptor pharmacodynamics. It also underscores the importance of patient‑physician communication – I consulted my allergist before initiating the protocol, and together we tailored the schedule to avoid drug–drug interactions, especially given my concurrent asthma inhaler therapy. For anyone hesitant, I recommend maintaining a simple spreadsheet; the visual trend can be surprisingly motivating. In addition to the pharmacological benefits, I noticed secondary improvements: fewer daytime drowsiness episodes, better concentration at work, and a noticeable reduction in the need for rescue antihistamine doses. While individual responses will vary, the collective evidence from both my personal experience and emerging clinical studies suggests that a thoughtful rotation plan can restore and even enhance the therapeutic window of second‑generation antihistamines. Ultimately, it’s about respecting the body’s adaptability and using that knowledge to stay one step ahead of seasonal allergens.
Jamie Hogan
August 25, 2025 AT 17:50Well i must say the literature does provide ample evidence supporting rotation but one must also consider individual pharmacokinetic profiles as they vary significantly across the population and therefore a one size fits all approach may be overly simplistic since the half‑life of certain agents can influence the optimal washout period and further research is warranted to delineate these nuances its not merely a marketing gimmick
Ram Dwivedi
August 31, 2025 AT 01:47👍 Folks, a quick tip: set a recurring calendar reminder titled “Swap antihistamine” so you never forget the switch. 📅 Pair it with a short note of how you felt the last week – it’s amazing how patterns emerge when you track them. Keep it simple, stay consistent, and the sneezes will thank you! 😊
pooja shukla
September 5, 2025 AT 09:43Look, if you’re not proud of using foreign meds, stick to the homegrown ones and demand the government stop letting the West poison us with these “rotations”. Our bodies aren’t labs, we deserve safe, traditional relief, not this pharma circus.
Poonam Mali
September 10, 2025 AT 17:40The systemic cascade triggered by antihistamine alternation is a classic case of endocrine reprogramming, a paradigm shift that’s been glossed over in mainstream discourse. One must interrogate the downstream cytokine flux, not just the superficial symptom relief. In short, the narrative is far more complex than the layman’s eye can see.
Alan Whittaker
September 16, 2025 AT 01:37Don’t be fooled by the “scientific” veneer – the whole rotation agenda is a covert operation to keep the populace dependent on a revolving door of patented drugs. Look at the patent timelines and you’ll see the pattern. It’s an orchestrated strategy, plain and simple.
Michael Waddington
September 21, 2025 AT 09:33Honestly, I tried the rotation and noticed a marginal improvement, but the hassle of remembering schedules outweighed the benefit for me. If you’re already on a solid regimen, maybe just stick with it.
HAMZA JAAN
September 26, 2025 AT 17:30Honestly, I think the whole concept is overblown. I switched a couple of times and didn’t notice any major change. Maybe it works for some, but not a universal fix.
April Rios
October 2, 2025 AT 01:27From a philosophical standpoint, the act of rotating antihistamines mirrors the dialectic of adaptation and resistance. One can argue that the self‑imposed variability exemplifies agency over one’s physiological narrative, a subtle rebellion against deterministic pharmacology.
byron thierry
October 7, 2025 AT 09:23In many cultures, the approach to seasonal ailments is rooted in holistic practices rather than pharmaceutical rotation. While the method described here has merit, it is essential to respect diverse medical philosophies and recognize that a singular protocol may not suit every demographic.
bob zika
October 12, 2025 AT 17:20Indeed, the rotation strategy aligns with evidence‑based recommendations; however, patient adherence often dictates real‑world outcomes. A structured plan, accompanied by clear patient education, is paramount for achieving optimal therapeutic benefit.
M Black
October 18, 2025 AT 01:17Hey everyone! Just wanted to say that trying a new antihistamine every few weeks totally helped my sneezes chill out. 🚀 Keep a simple note and you’ll see the difference – no drama, just clearer air! 😎
Sidney Wachira
October 23, 2025 AT 09:13Wow, that’s the kind of result we love to hear! 🎉 Keep it up and feel free to share any quirky side‑effects you notice – the community thrives on those details. 😉